The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…
News 4/21/09
Walgreen pharmacies fill a record 3.1 million electronic prescriptions in March, which is a 211% increase over the previous year. Still, this number represents only about 15% of all eligible prescriptions.
A Colorado doctor is found guilty of practicing medicine in California without a state license after prescribing an antidepressant over the Internet to a patient who later committed suicide. The patient had completed an online questionnaire, but the two never talked directly. The doctor has been sentenced to nine months in jail. His attorney says that, “Telemedicine is now dead,” since it is not feasible for physicians to be licensed in every state. Nice grandstanding, Mr. Attorney. Perhaps the conviction was for practicing without a license, but isn’t the bigger issue that the doctor was providing inadequate patient care, presumably with limited oversight?
McKesson kicks off its 11th annual McKesson Community Days, a program to bring employees together to participate in large-scale volunteer projects. Over 14,000 McKesson volunteers are creating care packages for hospitalized veterans at VA medical centers. The packages included a hand-written note of thanks, along with a fleece blanket and personal care items. Well done.
The administrator of the 16-physician Florida Heart Associates claims its transition to EMR has been worth the effort and cost because doctors are spending less time at work and reimbursements are up. The group took 12 to 18 months to review EMR systems and spent about $600,000 initially. After a two and half year transition, the group is now paperless. The administrator estimates the group now spends $11,000 to $14,000 a year per physician for support and updates. No word on which software they use, though it was supposedly developed by cardiologists.
Lee Memorial Health System (FL) and area doctors discuss interoperability and the exchange of patient data, a conversation that will undoubtedly be repeated in medical communities across the country in coming months. Even with the potential for federal funds, some community physicians are hesitant to partner with the health system and utilize Lee Memorial’s Epic system. Others wonder how they’ll be able to tie their existing EMR with the hospital’s system and who will pay for the connection. Everyone sees the value of connecting patient data, but today most communities lack a clear plan to make it happen.
Since launching its e-Prescribe Tennessee effort in December, the Tennessee Office of e-Health Initiatives has awarded $14.6 million in grants to 1,830 Tennessee providers. The $2,500 to $3,500 grants subsidize the cost of the required e-prescribing hardware and software.
A jailed Arkansas physician accused of illegally possessing of hand grenades sues state medical board members for persecution. Dr. Randeep Mann, who names both present and former board members in the suit, claims he was persecuted over the past six years, at least in part because he is Hindu from India rather than white, Christian, and native-born. Mann has been in jail since March 6 when he was arrested on firearm charges.
Federal agents raid two Indiana medical offices and three physician homes in connection with a Medicare fraud investigation. The raids follow a lengthy HHS investigation of two doctors affiliated with Doctor’s Hospital in Bremen. The physicians are suspected of billing fraud, improper referrals, and illegal kickbacks to physicians.
Sharp Community Medical Group (SCMG) in California announces that its first physician is live on the SCMG CONNECT EHR system. SCMG is working to establish a shared, single patient record for its 600 independent primary care physicians.
Top military doctors in Iraq aren’t happy with its new tracking system for wounded soldiers. The new system, Theater Medical Data Store (TMDS) replaced Joint Patient Tracking Application (JPAT). One of the main complaints involves data loading time (a minimum of three hours to load from the field and into servers in Virginia, and then to the physicians at medical centers in Germany.) Also a concern are the multiple information links for each patient, which make easy interpretation difficult. An army vascular surgeon sounds like his civilian counterparts: “I know JPTA is dead, but our current system is not functional. As we do more with less putting the administrative burdens on the doctors is ludicrous.”
A University of Texas School of Public Health study finds that the uninsured in Harris County are visiting hospital EDs for minor illnesses less often because of improved access to primary care programs and clinics. Over a three-year period, Harris County hospitals saw a 5.5% decline in the percentage of primary care-related visits to EDs by the uninsured. Diverting these patients to clinics saves an estimated $10 million per year.
Cardiac Science Corporation completes certification to connect its HeartCentrix ECG connectivity software to the Sage Intergy EHR.
The FTC issues a proposed rule requiring PHR vendors and related entities to notify consumers when their identifiable health data has been breached. Public comment is open until June 1.
The Vermont legislature explores the use of smart cards for health insurance, medical billing, and EMRs.
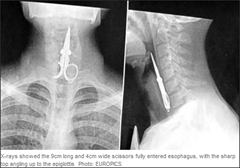
A Chinese man accidentally swallows a pair of nail scissors he was using as a toothpick. Doctors surgically removed the scissors, which had entered the man’s esophagus. If this had happened in America, you know this guy would have been asked to be the next spokesperson for Oral-B toothbrushes.


Not been the biggest McKesson fan, but the vets’ community service effort certainly puts a plus in their column. Thanks, McKesson peeps.