The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…
News 11/3/09
From Evan Steele: “Re: feedback to the government. The government has finally decided to listen to the physicians, upon whose participation the EHR incentives’ success depends. The HIT Standards Committee’s Implementation Workgroup launched a blog / Web site seeking feedback from practices regarding their experiences with EMR adoption, both bad and good. The results will be reported to the Committee on November 19th.” Comment here.
From Greg Anderson: “Re: flu clinic. Thanks so much for the kind link to my blog (via Chip Hart) about the H1N1 flu clinic at my wife’s practice last weekend. However, I wanted to correct two factual discrepancies. I am not the doctor — my wife (Susan Kressly, MD, FAAP) is. And, 18 hours is the amount of staff time we expended in total across all of the activities listed to give those doses. My good faith estimate is that we accomplished the total job in 1/3 to 1/2 of the time that would have been expended in the ‘average’ pediatric practice. To me, the key takeaway for the average observer is ‘look how much work doctors put into what seems like such a simple act, and look how little they get paid for this effort.’” Greg sent over another link that detailed an additional flu clinic’s activities on Halloween. The practice administered 145 flu shots to 114 patients in less than three hours. Based on what insurance is reimbursing, Greg calls the shot clinic a labor of love, and not a way for a pediatrician to get rich. He also adds, “Without an EMR, it has all the makings of a financial disaster, which is why some pediatric practices have elected not to participate in distributing this vaccine.” And, my apologies to Dr. Kressly (the witch in the picture above) for getting her title wrong last post.
Drummond Group, an interoperability test lab, announces that it will apply to become an EHR certifying body once ONC releases its requirements. I think mixing things up a bit and giving CCHIT some competition isn’t a bad thing. Of course it will lead to criticisms that one certification body is superior to the other and the bigger players will feel compelled to get multiple certifications jut to cover their bases. Will other entities step forward announcing they, too, intend to be a certifying body? Could be fun to see what unfolds.
With everyone focused on EMRs and how to obtain stimulus funds, practice management systems have taken a back seat. However, here’s a reminder of some of the basics that every PM system should include. The biggest question most practices likely have is whether to stick with one vendor for EMR and PM or go a best-of-breed approach. I have a bias to the one-vendor approach, primarily because it reduces interface costs and issues that can arise each time one or the other product needs to be upgraded. This AMA article also points out that providers should budget time and money for major hardware and software upgrades every three years, which I think is a wise suggestion.
Quality Systems’ Q2 numbers: revenue up 22%, EPS $0.41 vs. $0.37, meeting expectations on earnings and exceeding on revenue. ARRA is accelerating PM/EMR sales, the company says. Market cap for the company, including its QSI and NextGen divisions, is at $1.74 billion, of which founder and chairman Sheldon Razin holds over $300 million worth.
Athenahealth reports Q3 numbers: revenue up 37% to $49 million, EPS $0.14 vs. $0.14, missing expectations of $0.16.
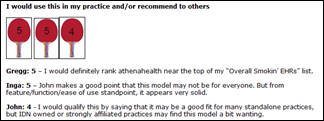
Speaking of athenahealth, I hope you had a chance to check out our overview of athenaClincals. Dr. Gregg Alexander, John Smaling of Vitalize Consulting, and I had a one-hour peek at the product and provided some of our impressions. Our goal was to go through the same general product overview that athenahealth would provide for a prospect, then comment on what we saw. It was not intended to be anything more than that, and thus did not include any detail on support, company background, client testimonials, etc. Our intent for this and and future overviews is to let people know what we perceive as the product’s strengths/weaknesses based on what the vendor shows us. Since it was our first one, I would appreciate your feedback. A couple of companies have stepped forward indicating they’d like to participate in our next review, so stay tuned. A special thanks to Gregg and John for their time participating in the demo and providing their impressions. Thanks also to the athena folks, who didn’t really know what they were getting themselves into when they agreed to participate. Incidentally, athenahealth is not a HIStalk or HIStalkPractice sponsor and did not provide us any sort of remuneration.
McAllen, Texas once again makes healthcare headlines. The area’s largest hospital system agrees to pay the federal government $27.5 million to settle allegations that it paid doctors illegal kickbacks to refer patients to its facilities. The government claims that South Texas Health Systems disguised payments to doctors in a series of sham contracts that included medical directorships and lease agreements.
Half of the doctors responding to a British survey say they are too busy typing into the computer to look patients in the eye. One doctor said, “The demands of the patient’s agenda, the Government’s agenda and the requirement that everything I hear, say and do must be meticulously recorded make for an extremely crowded consultation.”
HHS issues an interim final rule that increases penalties for HIPAA violations. The maximum individual penalty for civil violations jumps from $100 to $25,000 and the penalty cap grew from $25,000 to $1.5 million. Will The National Enquirer appeal?
Ambulatory healthcare clinics have had a total of 63 mass layoffs through the end of September, which is eight less than all of 2008. A mass layoff is defined as when at least 50 workers lose their jobs.
Score one for EHRs. CMS announces that in 2010, providers will be able to submit e-prescribing usage through qualified EHR systems or registries. In the past, providers were required to report e-prescribing based on patient medical claims. Providers will also be able to use their EHRs to report PQRI data. Next year’s payments will increase from 1.5% of total estimated allowed charges to 2%.