The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…
News 11/18/10
From Jimmy Bond: “Re: Practice Fusion. I have been wondering about Practice Fusion’s provider claims. They seem highly exaggerated. It will be interesting to see what happens to the company over the next year or so to see if they can sustain the free business model as well. They certainly have the hype part down well.” I have exchanged a couple of e-mails with Practice Fusion and have specifically asked for clarification on the provider count. Still waiting, but they seem open to talking about it. My opinion is that if Practice Fusion stands behinds its claims, it should be eager to show supporting data.
Allen Medical Group (CA) selects the Waiting Room Solutions EHR and PM for its multi-specialty, four-provider practice. Interestingly, the practice offers “off-premises medical services,” more commonly known as house calls.
Everything Channel’s CRN Magazine recognizes Aprima Medical Software as a top healthcare vendor. CRN’s list recognizes the top vendors with indirect sales channel programs; 30% of Aprima’s sales come through VAR channels.
Spring Medical Systems partners with Aqua Connect to provide secure remote access for SpringCharts EHR Mac customers.
Pennsylvania’s two RECs, PA REACH East and PA REACH West, designate eClinicalWorks, Sage, and Greenway, as group purchasing option vendors for EHRs. The RECs say they may add additional vendors to their list (don’t they always say that?)
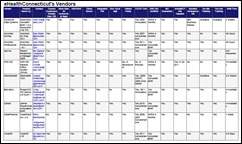
Speaking of RECs, I am fascinated by the various ways each organization labels its relationship with EHR vendors. I’ve seen vendors called everything from “preferred” to “pre-certified” to “group purchasing option.” Some RECs are establishing ties with 40 or more vendors. Others are taking a vendor-neutral stance and not affiliating with anyone. The above table shows all the EHR vendors that have been “qualified” by eHealthConnecticut. I like summary format they provide – it makes it easy to compare the vendors on various qualifications.
Covisint says its DocSite PQRI reporting registry was the highest-volume registry for 2009 with more than 4,500 successful submissions. Covisint is on track to help over 10,000 providers obtain 2010 PQRI payments.
Ulrich Medical Concepts teams with Intuit Health to give Ulrich’s EMR clients the option to use Intuit’s Health Patient Portal.
Something to ponder: by 2015, 500 million providers and consumers will use smart phone healthcare apps. Of the 17,000 mobile health apps today, 43% are designed for providers. And here I was thinking that smart phones would be obsolete by that time and we’d be obsessing about some completely new technology.
Verizon continues its efforts to be a player in medical data exchange arena, announcing plans to issue medical identity credentials to 2.3 million providers at no charge. The credentials will allow providers to receive digital health information via the Verizon Medical Data Exchange and access a variety of IT tools and applications, including EMRs and electronic prescribing services.
eClinicalWorks says nearly 3,000 people attended its annual users conference in Orlando. The event took place over Halloween weekend and the company encouraged users to bring their families. More than 500 family members participated, including kids who had a chance to wear their costumes and trick-or-treat throughout the exhibit hall. eCW also set up a costume station so everyone could find the perfect fashion accessory (sorry I missed that!) I’m not sure what what look CEO Garish Navani was going for in this photo (a superhero cowboy, perhaps?) but he and his cohorts look to be having fun.
Based on feedback from 2.7 million patients, Press Ganey concludes that patients who spend less time waiting to see their provider are more satisfied with their office visit than patients having longer wait times (d’uh!) Patient satisfaction was also tied to the sensitivity of the caregivers to patients’ needs, the overall cheerfulness of the practice, and the overall rating of care. Interesting data point: patients waited an average of 30 minutes to see their neurosurgeon and only 17 minutes to see their optometrist.
Police in Boise, ID arrest a woman for posing as a plastic surgeon and performing breast exams in bars on at least two women. Following the evaluations, the women were given a phone number to a legitimate plastic surgeon in town. Police got involved when the surgeon’s office called to report several women calling in reference to setting up appointments with the fictitious doctor. Readers, make your own assessments.
SRSsoft CEO Evan Steele and I exchanged e-mails on Meaningful Use for specialists. I asked him to write up his thoughts.
Thoughts on Meaningful Use Challenges for Specialists
By Evan Steele
The final Meaningful Use rule, released in July, included a provision for excluding Meaningful Use measures that don’t apply to a physician’s particular practice, but many were either unaware of this provision or were skeptical about its application. Since SRS predominantly represents specialist physicians, I was very encouraged by David Blumenthal’s recent confirmation of this provision to the American Academy of Ophthalmology. His comments were reported earlier this week in American Medical News in an article by Pamela Lewis Dolan, “HHS Spreads the Word about How Specialists Can Meet Meaningful Use.” The subtitle is “One way is to claim exceptions because the guidelines don’t apply to their specialty.”
According to the article, Dr. Blumenthal is telling physicians that “there are plenty of exceptions…” Plenty may be a bit of an overstatement since any individual physician will likely be eligible for only a few of them, but his comments should be taken as a positive indication of the government’s interest in the participation of specialists. It is encouraging that CMS added this flexibility to what is basically a primary-care focused set of measures since measure excludability eliminates some of the participation obstacles faced by specialists. Going forward, what I hope the government will focus on is defining Meaningful Use so that it is meaningful to specialists and relevant to the care they deliver.
To clarify the exclusions, it should be noted that it is not quite as simple as merely claiming an exemption because a particular measure doesn’t apply to one’s specialty. The regulations state that a provider can only exclude a Meaningful Use measure if that measure is specifically identified as excludable (as six of the 15 Core Set Measures and seven of the 10 Menu Set Measures are), and further, if the provider attests to meeting the criteria for exclusion.
It is likely that most specialists can reasonably claim as “not relevant to the scope of their practice” only one of the Core Measures, but it’s an important one in terms of impact on their productivity: recording vital signs. Ophthalmologists, orthopaedists, and dermatologists, for example — many of whom do not even have a blood pressure monitor in their office — are not expected to add blood pressure monitoring to their workflows. This modification successfully addresses one of the concerns related to the impact of meaningful use on specialists.
In addition, although they cannot technically “exclude” reporting on clinical quality measures, specialists can report zeroes for both the numerator and the denominator of the required quality measures if none are appropriate to their practice. This will be very helpful to specialists like dermatologists, for whom the regulations contain no relevant quality measures, and orthopaedists, for whom there are only one or two that might apply. Excluded measures translate to less work for the physician since these measures do not have to be replaced by others.
Although clarification is needed on some issues — for example, whether the physician will be the ultimate arbiter of eligibility for a particular exclusion — the fact that David Blumenthal is putting his voice behind how the regulations apply to specialists is a very positive sign for the future.




Regarding MU challenges for specialists: I am so tired of hearing that specialists can’t take vital signs and that it impairs their productivity. News flash, if you are prescribing medications, you should be monitoring some things, folks. Especially you orthopedists that chock my elderly patients full of NSAIDs and COX-2 inhibitors that tip their CHF over the edge. Maybe a pulse and a BP would be a good idea, eh? And monitoring height and weight to see if those elderly patients are having occult vertebral compression fractures or to counsel them on their elevated BMI being a risk factor for surgery? And ophthalmologists? Remember that Timoptic can cause cardiorespiratory issues and has caused death in bradycardic patients? Maybe a pulse check would be a good idea. Especially with the availability of interfaced vitals capture devices for your EHR (that can do 5 vitals in less than a minute) it might be time to check a few vitals. And not to avoid picking on the dermatologists, don’t forget, tons of the diseases you treat have systemic components and some of your meds are super-toxic. Don’t get me wrong, I don’t expect you to inquire about helmet use in bike-riding tweens or which way the baby’s car seat is facing, but vital signs are clinically relevant to everyone and not just a productivity-imparing nuisance. Maybe for this one I should have signed it as “semi-bitter PCP in the trenches.”
The REC news continues to be interesting (to say the least). I wonder how long these preferred vendor lists will last once HITECH really picks up speed and more software becomes certified. Also, it’s tough to know how RECs will handle physicians if they become dissastisifed with their EHR and want to switch.
Speaking of EHR satisfaction, a new website opened this week called EHR Event, soliciting info on problems providers have had with their system. I wrote what little I could find over at our blog (where we’ve got a nice round of comments going). There’s still a lot that’s unclear about the website and its mission: I wonder if you and Mr. H could give it the HIStalk go over, maybe sniff some inside info out?
re: Meaningful Use measures that don’t apply to a physician’s particular practice
Just wondering if anyone out there may have developed a matrix of sorts that identifies, by specialty, which measures might not apply and be excludable. If so, I’d love to see it!
Thanks!