The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…
News 6/16/11
HHS’s Office of Minority Health and Quest Diagnostics announce a program to donate approximately 75 MedPlus EHR user licenses to physicians in small practices serving minority populations in Houston. The initiative includes subscription fees for 12 months and educational assistance from the University of Texas Health Science Center at Houston REC.
Hanger Orthopedic Group will deploy NextGen Ambulatory EHR and PM at its 675 orthotic and prosthetic patient care centers in 45 states.
PDR Network launches RxEvent, an online network to collect and distribute adverse drug events. The service is targeted at prescribers, who typically don’t report adverse events to the FDA because it is too time consuming. Greenway Medical, athenahealth, and other ambulatory vendors will be integrating the RxEvent reporting into their EHR applications.
Pinehurst Dermatology (NC) contracts with SRS for its EHR solution.
ABEL Medical Software announces a OEM program for resellers interested in selling its ABELMed EHR-EMR/PM product.
Mitochon Systems partners with CollaborateMD to offer Mitochon’s free mEMR product with CollaborateMD’s PM solution. Like Practice Fusion, Mitochon’s model displays ads within the application’s workflow. Meanwhile, CollaborateMD claims a solo physician can spend as little as $7 a day for unlimited claims processing, electronic remittance, and patient eligibility. Call me a skeptic, but I have to wonder what’s missing in that $7/day solution that includes EMR and PM.
NaviNet introduces NaviNet Mobile to allow pharmacy benefit managers to deliver patient medical information to physicians via handheld devices.
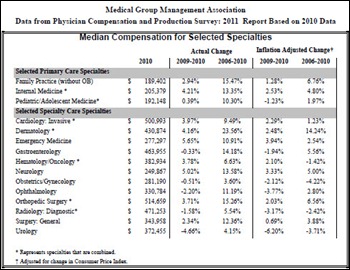
Physician compensation grew for some specialties in 2010 and decreased for others. For example, emergency medicine compensation increased 5.6%, while urology income fell 4.66%. Median compensation for family practitioners was $189,402; invasive cardiologists averaged $500,993.
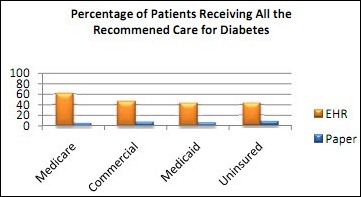
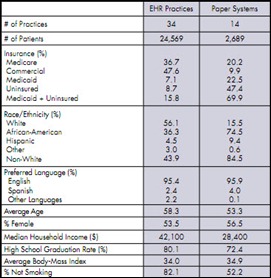
A Robert Wood Johnson Foundation report finds that 51% of office-treated diabetics in Cleveland received all the care they needed from practices using electronic medical records vs. 7% from paper-based practices. A similar correlation was found for diabetic outcomes. Mr. H mentioned in HIStalk not being able to find the study methodology, but I dug a little and found this report by Better Health Greater Cleveland. There is a fair amount of difference in the demographics between the EHR practices and the paper practices, with the paper practices including a heavy number of non-insured and Medicaid patients (69.9% compared to 15.8% of the EHR practices.) The paper practices were also twice as likely to have non-white patients (86.5% compared to 43.9%.) When you take those facts into consideration, the EHR-diabetes care correlation does not seem as strong.
In 2009, the number of paid malpractice claims reported in the outpatient setting was similar to inpatient numbers, suggesting medical mistakes are almost equally common in the two settings. The authors of the NEJM-published study recommend more patient safety efforts in the outpatient setting, including the implementation of e-prescribing systems and EMRs.
HIMSS Electronic Record Health Association (ERHA), a trade association of 46 EHR vendors, submits generally favorable comments on the proposed ACO rules. No doubt the opinion was influenced by the EHRA’s acknowledgement that ACOs will require robust IT infrastructures. The organization recommends that CMS reduce the required threshold for EHR meaningful use providers from 50% of primary care providers to 25% of all EPs. In addition, EHRA urges CMS to reduce the requirement for quality measurement reporting from 65 items to 20 or fewer.