The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…
News 4/1/14

The one year delay for the mandatory implementation of ICD-10 is almost a done deal following the Senate’s approval of the legislation on Monday. The bill primarily addresses a Sustainable Growth Rate fix that prevents a 24 percent reduction on physician Medicare payments as of April 1 and will now go to the President for signature. I wonder how many of the 535 voting members of Congress had a clue that the legislation included the ICD-10 date change, much less understood its potential impact to the industry. For all the gloomy predictions about disruptions in cash flow and lack of readiness by various stakeholders, shifting the deadline will come with a whole new set of issues and expenses. For example, what about all the ICD-10 ready software releases that likely include unrelated enhancements? Will vendors have to invest more money to re-engineer updates so that the unrelated enhancements work with ICD-9? And then there is the question of how we can wait one more year without having a specific code for things like being hit by an object falling from an aircraft (V96.31XA) or for an injury caused by a sea lion bite (W56.11XS).
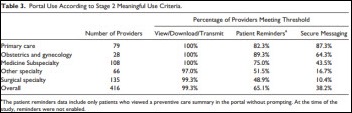
Specialists who are late in adopting EHRs may struggle to meet the patient portal requirements to satisfy Stage 2 MU requirements, according to a study published in the American Journal of Medical Quality. Researchers found that 87 percent of primary care physicians would have met the email communication threshold for Stage 2 in 2013, but only 37 percent of specialists, probably because specialists that don’t provide chronic care generate fewer emails. The authors conclude that other avenues of patient engagement, such as providing patient education or online post-op instructions, would be more appropriate for specialists. This particular Stage 2 requirement is just one of several that is well-intentioned but difficult, if not unrealistic, for specialists to achieve. Is it any wonder that a significant number of specialists are predicted to “drop-out” of the MU program before attesting for Stage 2?
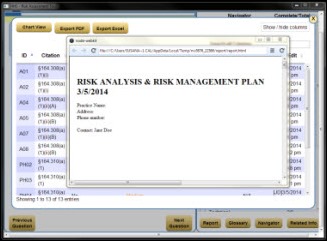
HHS releases a security risk assessment tool for small to medium physician practices. It’s available for the desktop, iPad, or as Word documents and produces a report that can be provided to auditors.
Insight Software will integrate DrFirst’s Rcopia e-prescribing platform into its My Vision Express EHR.
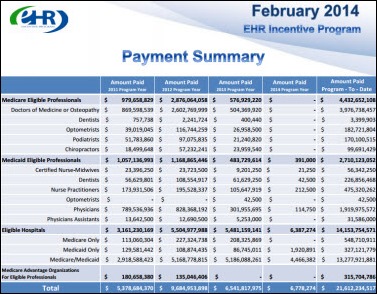
Through February, 2014, a total of 343,204 EPs have been paid $4.4 billion in MU incentives under Medicare, $2.7 billion under Medicaid, and $315.7 million under Medicare Advantage.
From across the pond: 60 percent of GPs in European Union nations were using eHealth tools in 2013, a 50 percent increase since 2007. Interoperability issues, a lack of regulatory framework, and inadequate resources are some of the most common barriers to adoption (sound familiar?) The Netherlands, Denmark, and the UK led other nations in efforts to digitize patient records.
Best Doctors, which offers remote second opinion services, launches Medting, an online physician collaborative platform that allows doctors to collaborate to make correct diagnoses and to seek guidance for patient treatment plans.
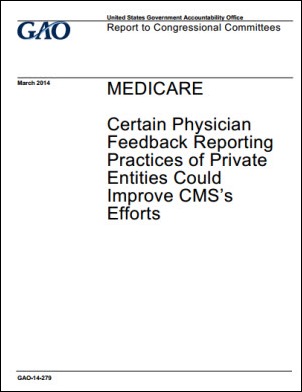
The Government Accountability Office recommends that CMS expand performance benchmarks that assess Medicare physicians to include state or regional averages. In addition, as CMS implements and refines its physician feedback and Value Modifier programs, it should follow the example of private entities that use multiple benchmarks and should disseminate feedback reports more frequently than once a year.
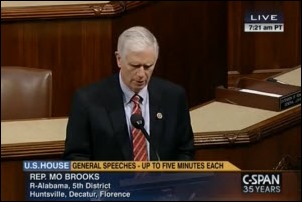
An Alabama legislator reads a letter from constituent Marlin Gill, MD, who clearly is not a big fan of Washington and its “war on doctors.” I wonder how many other physicians share his views and believe all the government’s various initiatives to improve quality and trim costs is wasted effort. Among his list of complaints:
- Being “forced by ill-informed bureaucrats to implement electronic medical records” that cost is four doctor practice “well over $100,000 plus continuing yearly operational costs . . . all of which does not help take care of one patient while driving up the cost of every patient’s health care.”
- “Destructive regulations” that add costs and “force doctors to focus on things other than patient care and reduce the number of patients we can help each day.”
- The cost of migrating to ICD-10, which is costing his practice $80,000 “without one iota of improvement in health care quality.”
Email Inga.