The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…
News 12/14/10
The cost to adopt an EMR may be as much as $120,000 per physician, though it can reduce overall costs with full implementation and accelerated workflow. This report suggests that during the first year of adoption, physicians may manage 10% fewer encounters. As a result, lost revenue is a bigger drain on a practice than the actual EHR software and hardware costs. The methodology for this study is a bit questionable (findings were largely based on a survey of 200 practices that had not yet adopted EMRs), but, I agree with the bottom line assessment: the sooner the implementation is completed, the sooner the returns will be be realized.
I’m guessing this doctor might concur with the above findings. Dr. Paul Meriwether, a small-town family practice doctor, shares with the local paper his struggles implementing a new EMR. Dr. Paul Meriwether says he and his partner added 2.5 FTEs and still had to reduce their patient load by 30-50%. Though he considers the EMR “a natural evolution of the nature of healthcare,” the road hasn’t been easy:
As we get used to the system, the adjustments are limiting us – limiting the number of new patients, because they take longer to enter into the system. Everything has to manually be put in to the computer. We’re hoping six months from now, we will be back up functioning like before… I believe once we get it into the computer and it’s in the system, it’s going to get better. We were told this, but it is very frustrating. It’s something, I’m sure, like, 30 years ago, things were implemented that doctors hated to do, but that now is second nature for them.
Marshfield Clinic (WI) will receive a $16.5 million performance payment based on achieving 100% of benchmark performance measures in CMS’s Physician Group Practice Demonstration. Marshfield calculates it has saved over $83 million in its first four years participating in the national demonstration project designed to incent practices to improve quality of care. Dr. Theodore Praxel, the clinic’s medical director for quality improvement and care management, says that initiatives such as a 24-hour nurse line, anticoagulation program, heart failure care management program, and EMR were integral to the cost savings. Four other group practices will also receive bonuses as part of the demonstration project, for a total of $31.7 million. A similar demonstration project for solo and small practices will pay $9.5 million to more than 500 practices.
The AMA and 103 state and specialty medical societies urge HHS to revise the Medicare e-prescribing penalty policy and better align it with complete EHR incentives programs. The policy penalizes physicians in 2012 and 2013 if they don’t e-prescribe in the first six months of 2011. The AMA says this policy will hurt practices that are implementing complete EHR systems. To participate in the 2011 e-prescribing program, some physicians may have to spend additional resources on an e-prescribing program that may be discarded once the physician moves to a complete EHR.
Healthcare Partners Medical Group, a 1,200-physician primary care group in California, goes live on Unity RIS/PACS from DR Systems.
ICSA Labs and SLI Global Solutions join CCHIT, Drummond, and InfoGard as the latest ONC-ACTBs. Neither of the new companies mention the EHR certification program on their websites (yet).
RCM provider ZirMed raises an undisclosed amount of venture backing from Sequoia Capital.
McKesson names Professional Data Services its Practice Partner Value-Added Reseller of the Year for the fifth straight year.
WellDoc announces integration of its DiabetesManager solution into a “leading” EHR solution, which I am told is Allscripts.
Consulting firm Surrex EHR Solutions partners with gloStream to provide sales and implementation of the gloStream platform.
Clinical messaging provider Kryptiq ranks number five on Portland Business Journal’s list of Oregon’s Most Admired Technology companies, based on the votes of 1,800 Oregon CEOs.
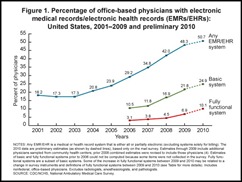
A CDC survey finds that around half of physician practices use EMRs, but only 25% of practices use a system that meets “basic system” functionality, with just 10% using a “fully functional” EMR that includes medical history, drug interaction checking, e-prescribing, electronic ordering of lab and radiology tests, and viewing electronic images. Still, the use “fully functional” EMRs has gone from 3.1% to 10% since 2006. Laggard states include Kentucky, Louisiana, and Florida, in which more than 60% of physicians in practice do not use any form of EMR. Leading the pack is Utah, with 51.5% of office-based doctors having access to a basic EMR.
Meanwhile, a 2011 Black Book Ranking’s user survey suggests that 90% of providers that have purchased EMRs aren’t ready to meet Meaningful Use implementation goals. The top reasons users cite for delayed implementations included lack of support from vendors, cost for additional vendor or consultant support, and lack of properly trained staff. Another noted problem that sounds like a great catch-all excuse to blame “others”: a hurried selection of an EHR vendor that resulted in negative consequences.