Chet Speed is vice president of public policy at American Medical Group Association of Alexandria, VA.

Review the concept of Accountable Care Organizations.
The ACO law was patterned after a demonstration project that was going on at CMS. It was called the Physician Group Practice Demonstration, kind of like a P4P demo. That was a five-year demo. It included 10 sites. Out of those 10, nine were AMGA members. It included standalone group practices, a couple of automated delivery systems, and even a hospital MSO.
Later, the way the law evolved was we had a few of our members in the PGP demo present some of their experiences to the Hill staff. The Hill staff was looking for delivery systems for healthcare reform and they asked us to draft the first draft of the ACO statute. The important thing is that if you’re really looking for a model of pre-existing ACOs, the PGP demo is a place for them to look.
The PGP demo essentially had two components to it. One, it had a component to improve quality. It had one to provide some savings in the Medicare program. In a macro sense, all 10 PGP demo sites met the quality metrics. On the cost side, they have to produce cost savings. One of the obstacles to actually making money under the PGP was you have to save 2% off the top before you start ensuring savings. So, only five out of 10 groups actually made money, so to speak, on the PGP demo.
What’s the the elevator pitch for ACOs?
It begins to transform the volume-based, fee-for-service reimbursement system because you do have to hit your quality metrics. And, you do have to be able to produce some sort of a cost savings. This cost savings can’t be the classic churn-and-burn fee-for-service. And to ensure that it’s not just all cost savings, you have to hit quality measures.
If I’m a provider, what’s the advantage of participating in an ACO?
It depends on what kind of provider you are. If you’re an AMGA member and or you’re integrated delivery system like Henry Ford or Ochsner or you’re a standalone practice like Mercy Clinic in Des Moines with 130 docs not affiliated with a hospital, I think the benefits are that your group has already invested a lot of the infrastructure that’s required to: one, improve your quality; and two, hit your cost savings requirements.
In both, I think with that infrastructure, typically, you have primary care industry docs under one roof. You’ve got allied health professionals that do the real care coordination, like your nurses, diabetic managers, etc. Also you invested in the EMR system. I think 85% of our members either have an EMR system up and running or are implementing one right now. If you have that infrastructure in place, you’re actually ready to meet requirements and potentially share in savings paid to you by the Medicare program.
But you indicated only half of the practices in the demo project actually got to take advantage of that savings. Is that right?
Yes, that’s right.
What needs to be tweaked in the model?
That’s a great question, and that’s what everyone’s actually asking. Right now, the statute’s fairly broad like all laws are, and where the rubber hits the road is right now in CMS’s hands. They have to draft the regulations that implement the law. Depending on how those regulations are drafted, you could have a very attractive ACO program or you could have one that doesn’t attract a lot of people at all because some of the things that they have to answer.
So the question you have to answer is, for instance, what is that savings threshold going to be? I know P4P was 2%. The law says that the threshold is pegged at the amount of Medicare beneficiaries you have. So if you have 30,000 beneficiaries if you’re a large group, does that mean your threshold is 2%, 1%, or 0.5%? Depending on what the threshold is, you’re going to get people to join or you won’t get people to join.
Another important question — this all stems from the PGP experience — is patient attribution. You need to know who your patients are so you can measure yourself. You need feedback from CMS on a timely basis so you know how you’re doing with those patients on cost and quality. Because without knowing, you can’t re-engineer your care and management processes to take advantage of this; to either redo or keep doing, depending on the result. What is the shared savings percentage going to be? Under the PGP it was and 80/20 split — the PGP folks got 80% and CMS got 20%. So what are the ACO splits going to be — 80/20, 50/50?
That’s policy related to the ACO threshold issue. You need to have a workable threshold and you need to have a decent shared savings split. Those financial issues are going to be very important.
Will it be mandated how the funds will be distributed within a particular ACO?
The statute basically says ACOs have to have a legal structure that allows them to make and distribute payments. That’s all it says. I don’t know how deep a dive CMS is going to do to how the ACO decides to distribute payments. That seems a little prescriptive.
Let’s say you’re an integrated delivery system. Obviously, legally, you can accept the shared savings amount — let’s say its $10. Then internally, you’re going to make distributions based on an internal plan. That could be at the department level like internal medicine or endocrinology or gastro or cardiology, etc. I think the question’s really up in the air on how the distributions are going to be made.
If CMS essentially says, “Do as you wish,” then it really will be up to the individual provider. That becomes a little trickier if you have say, a group practice and a hospital that aren’t integrated but joined together to be an ACO. That does become tricky. So who does CMS give the money to, the group or the hospital? And once that decision’s made, say we’ll give it to the group, and then the group and the hospital have to decide themselves how that money gets split.
Then let’s say you have outside providers. What if you have a skilled nursing facility that you included in your ACO because you want to take care of the post-acute population? Then you’ve got to figure out, OK, how many patients go to this facility?
Let’s say that you have a neurologist that’s not part of the practice that’s a solo doctor. Theoretically, that neurologist could be part of the ACO. Is that correct?
Absolutely. It’s this hospital medical staff idea that’s the Elliot Fisher model, with ACOs basically being formed out of one community hospital and its medical staff. Say it’s like Sibley Hospital and 100 docs in the northwestern Washington, DC community. How do you distribute payments then becomes very tricky because nobody’s really organized under one tent. You know it’s one hospital administrator and 100 different physicians and there’s not always a cultural cooperation between your community hospitals and community docs. So that’ll be a tricky scenario.
We don’t see a lot of that here because our folks are fairly organized, but that will be interesting.
Who’s going to make that call? Is it going to be a progressive group practice making that, or a progressive hospital system, or is it going to be mandated? What’s your thought?
You mean from CMS’s point of view or just what the market will do?
Both. Will CMS decide to call the shots or will it let the market make that call?
I hope CMS lets the market make those calls. Like I said, the statute’s fairly broad. I hope CMS doesn’t say, “The ACO shall distribute payments based on…with this methodology,” etc. You know, “Just pick something,” I hope they say, “The ACO shall make and distribute payments as required by law” and leave it up to the individual ACO. Within our membership it’s a little easier because it’s organized for the most part.
In an unorganized community, that becomes pretty darn difficult, I’d say, because you really have to have a lot of trust between the community docs and the hospital administrator who will probably receive the money in that type of model.
It seems to me the one that doesn’t win from this model is the solo physician. Or a small physician group won’t because they lack the infrastructure and organization necessary to participate. Is that just the way it is, or is it going to force more consolidation? What’s your impression?
I think when Congress drafted this, they focused on increasing the provider integration. They’re looking at organized group practices as a better way of delivering care. They’re actively looking at care coordination, which is lacking right now in the system, and you get more care coordination from these more integrated delivery models. So I think it’s safe to say that if you’re a solo doc, you’re going to have a much tougher time being part of an ACO than if you’re a doc working at Mayo, for instance.
I think you’re hitting the right thing. Congress does want doctors to become more organized because the evidence is showing that the quality, at least, is measured better in more organized systems and the costs are less. I think Congress paid attention to that.
Do you think could be possible that ACOs become closed systems and refuse admissions for providers whose performance metrics are not at a pre-determined level?
Like an ACO credentialing?
Right.
Yes, I think that’s a good question. I hadn’t thought about that, but I think if you’re a physician whose quality is substandard, I’m sure they can say no. There is no requirement in the law that says you must take anyone. So yes, it can be closed.
Actually the groups that I talk to actually want to increase the number of doctors, not necessarily that they employ, but, they want to let more doctors be in a panel, for lack of a better word, than less.
So do you think that, in time, there will be competition for these providers? Let’s say that there are multiple hospital systems with ACOs in a particular region. Do you think that they’ll compete for physician participation?
Yes, I think so. If you’re a community and there’s four hospitals and a couple of organized groups and unorganized community doctors, I think you’re going to see a couple ACOs being developed, sure. And they are going to compete.
How will they compete? How will they differentiate themselves financially to providers? If I’m a neurologist, why do I want to become part of your ACO versus the one down the street?
I think probably whichever you feel is more financially stable and has those better quality platforms. You know, most physicians admit to one hospital because they think the care’s better there. I guess at some point it’s just more convenient, but I think the better providers typically win out in these situations.
I can think of an area in Maryland where there are a couple of hospitals and one just is much better than the other because the doctors view the quality at that hospital as higher than the other. I think that’s probably what will happen with ACOs.
What type of IT infrastructure would be required to meet the quality reporting requirements and satisfy coordination of care needs? Are EHRs a necessity and what other tools do are needed?
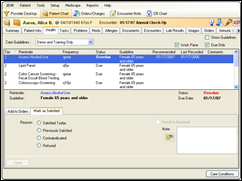
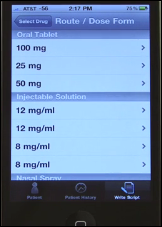
I think an EMR is a core necessity. And, as I talk to some of the really smart HIT people, what they say is that if you use your EMR just as, literally, an electronic medical record, you’re wasting 80% of its value. You have to use the EMR as, first, a data collection tool. Obviously, to be measured you have to collect the data and then submit it.
Another critical aspect is the analytical capabilities of the EMR system. Obviously, if you’re going to determine appropriate practice patterns, you need to look at the data that’s input in the EMR and analyze it. For instance, if you have 25 primary care physicians and they all have a number of diabetic patients; and 22 out of the 25 have an appropriate A1C levels and three do not, you need to be able to look at the data and say, “OK, why are those three clinicians not doing as well as their colleagues’?” And presumably, through the EMR you can see, oh, OK, they’re not doing required protocol.
On the other hand, perhaps they’re just the best thought-of physicians and they get the harder cases. But being able to analyze the data which you collect in the EMR is critical to understanding situations just like that.
What else do I need to know?
A lot is alive around ACOs right now. You can say anything you want about ACOs, really, and you’re probably right. That’ll start to be narrowed when CMS comes out with its proposed regulations.
Which will be when?
This fall? I heard September to the end of the year. Once they start to answer some of these questions, that’ll provide a good indication of how successful this program may be.
Are ACOs something to be feared or something to embrace?
I hope it’s something to be embraced, but we just don’t know yet. I think the commercial payers are also intensely looking at ACOs. Obviously, they see savings, particularly on the hospital side, that come along with quality improvements. So I think the commercial payers are going to look at this model and probably pilot it a little bit to see if it’s workable.










The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…