HIStalk Practice Interviews Jeffery Daigrepont
Jeffery Daigrepont is senior vice president of Coker Goup.
Give me some background on Coker Group, as well as your background.
We’re very much a traditional consulting firm. We have two segments. One is more operations in nature, where it deals with a lot of strategy work for hospitals and physician practices. Then we have a technology division, which I head up, which is strictly focused on IT strategies.
Where we’re a little bit unique is we do not have any financial ties with any vendor. We’re 100% non-biased and we work with a lot of folks, largely on the procurement, but also implementation. Believe it or not, about 30% of our projects are removing failed EHR systems, or going back in and reinvigorating EHR systems. That’s kind of it in a nutshell.
How long have you been with the company?
I’ve been with them ten years.
How do you see healthcare reform and ARRA complimenting one another? Or, do you think they actually conflict with one another?
I believe most doctors see reform — at least in the way it was passed recently — as a negative thing, with ARRA already being passed. I believe in order to survive they’re going to have to build better mousetraps, which means that to offset a lot of the reductions or the need to be expected to see more patients that’s now going to be covered, doctors are going to have to become more efficient if they’re going to survive.
Obviously, for those of us in the industry, it’s probably going to help us because we would be available to assist those and become more efficient. While some doctors see reform as negative, I also think now that it’s becoming passed, there’s a little bit of a sigh of relief. I’m not sure, but I’m wondering if now people will start moving on and making decisions. I think for a long period of time people were kind of putting major decisions off waiting to see exactly what it was going to look like and how they were going to be affected by it.
So are you seeing an uptick in practices moving forward with adoption?
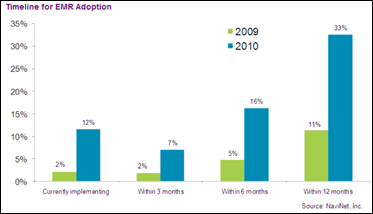
I will say that when ARRA first came out, there was a lot of uptick in being intrigued and renewed interest. The market was kind of reinvigorated, so conferences saw an increase in attendance. I saw a huge uptick in doing interviews, speaking, presenting. A lot more people were coming to attend lectures on vendor selection and things like that. The market was upticked, but what I didn’t see a spike — I didn’t necessarily see a spike in the actual execution of contracts. There was a lot of interest whirling, but I think everybody was putting off the actual signing of the contracts.
Now, what was interesting; this week alone, I’ve seen a pretty considerable increase in past clients that were either on the fence or waiting to do something that said, “OK, we’re ready to begin thinking real serious about this, and ready to start moving forward.” I don’t know what that percentage is. It may just be a fluke, but I do think many people have delayed major decisions until they saw exactly what was going to happen.
What impact do you think the RECs will have on the industry?
That’s a good question. First off, they have to be financially sustainable. Really, the only value that I see, at least on the surface, is to assist with implementation. So on one hand, that’s a pretty good source of revenue for the vendor. The vendor has to decide how much of that they really want to share with the Regional Extension Center, and whether or not there is enough room.
Then, once you do the implementation, what other tricks do you have? I mean, the vendors at least have recurring revenue for annual maintenance and support, and whatnot, so they can be sustainable. We do implementation and our clients are like, “How soon can you get here? How soon can you get it done?” They do not want people camping out on their payroll for an indefinite amount of time.
The other thing that I’m concerned about is whether or not there’s opportunity for conflict of interest. Let’s say Vendor A has a larger margin and is willing to share more in that margin or give up portions of the services that would ordinarily be done by the vendor, or through other strategic relationships — so hey, we’ll tilt business your way to the REC. Does that then induce more referrals or more friendliness from the Regional Extension Center to that particular vendor that wants to share more of their revenue, versus ones that might price their services a lot leaner and won’t have as much margin to share with these folks?
Then you also have the question of subject matter expertise, as to how deep will the vendor go? Because at the end of the day, the vendor’s name and credibility will be on the line. I know from doing a lot of project management and implementation work, there’s always a fine line between “I recommended this vendor,” and then I show up and do implementation services. If you screw up the implementation services, you can easily get upside down with both the vendor and the health system. Then who’s accountable?
One of the things you see vendors having to do all the time is go back in and redo stuff because, “Hey, I got bad advice. The trainer was a bonehead. This was just a total screw up.” The vendor has the value of the long-term relationship, so they’ll usually suck it up and go back in there and redo it. If one of these Regional Extension employees go in and they muck it up, who covers the note for them to come back in and do it a second time? I don’t know, contractually, who’s made accountable either.
I think the best model that I would think that could play out — and I don’t know how deep RECs would want to go, but every project has vendor-side responsibility and client side responsibilities. I think one of the big areas of need right now is client-side responsibilities, because they don’t have good project managers/leaders. So, the Regional Extension Center could play the role of the advocate for the clients, versus playing the role of the vendor. They’re going to have to decide if they’re going to be the client’s advocate, or they’re going to be the vendor’s go-to resource for delivering the services. You really can’t be both.
Obviously, because the RECs can’t be experts at every last software, they’re going to narrow down their preferred vendor list. What do you think is going to happen to those companies that don’t make that short list?
That’s what I was saying. I think if you’re forced to create a business model where you have to be financially sustainable, then human nature’s going to dictate that those Regional Extension Centers’ preferred vendors are likely going to be those that have the most opportunity.
I’ll give you a real good example. A lot of the little vendors, Web-based ASP vendors, are very light and nimble. They’ve got their implementation down to a couple days and they’re usually attracting physicians that really don’t want a lot of heavy implementation. Just keep it short and sweet. A lot of tools built, baked into the product so the product can self-customize and whatnot. When one of our clients goes that route, and we’re perfectly OK with it, there’s less opportunity for us to provide additional services.
Whereas, if they buy a NextGen, an Allscripts, if they buy an Epic, we’re in there for the next five years. It’s that heavy of a system. So, if I was building a Regional Extension Center and I need recurring, sustainable revenue, I’m naturally looking at a system that might be a little bit more self-serving. That gives me the opportunity to provide more services versus a light vendor.
So, I do think it’s going to hurt the smaller business that have been innovative, and trying to get their products installed in a way that doesn’t require a whole army of workforce.
I know you’ve worked with a number of hospitals to help them align with physicians. What are some creative ways for hospitals to do this?
I think that’s a great model, because many of the hospitals can subsidize a good portion of the cost, and usually care is a local thing. So when they can collaborate and become clinically integrated, there’s a lot of value. I think, conceptually, it’s a model that saves all the stakeholders a lot of money, and I also think it improves the interaction between the hospital and the physician, as well as with the patient.
The challenge with the model, almost always is politics — control of data and boundaries. If a hospital wants to buy Allscripts and then distribute it to their medical staff, Allscripts will continue to sell directly to that medical staff as well. You really have to be proactive in getting an understanding with your vendor that you are going to take their HIT system to market; and rather than unintentionally competing with your own vendor, work out more of a collaboration strategy where they help promote it so there’s not that market conflict.
Now some vendors like Epic, for example, have what they call their “hub strategy” and they’re actually teaching their hospitals and consulting with their hospitals on how to deliver Epic to the community. Epic doesn’t want to fool with small practices, but they’re more than willing to help prop up their hospitals to do it.
The ones that really do it right — Sentara Health System is a good example — where they really kind of commercialized their IT services. They even branded it with its own name. It’s called eCare. Well, eCare’s Epic, and the hospital, Sentara. But if it appears to be something kind of unique and not just the hospital giving me an EHR system or sharing it, it tends to play out a little better.
Also, another good structure, or the governance structure, is to include a lot of stakeholders or different members of the party you’re governing. Because you’re dealing with things that typically a hospital doesn’t have to address, they’re on one hand trying to stay a hospital, but they’re also becoming a vendor.
I’ve seen cases where the hospital gives an EMR system to a practice and that practice implodes. Well, the two doctors now don’t get along in the practice, and they’re both fighting over who owns the records. The hospital’s caught in the middle, so you’ve really got to work out a good service level agreement between your hospital and your medical staff or you could really get into some very uncomfortable situations.
What would you say some of the biggest mistakes practices make in the EMR selection and implementation process?
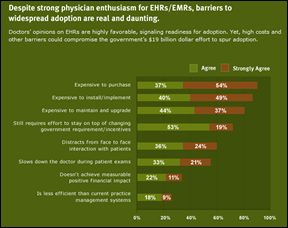
Probably the biggest one — and it’s really, more often than not, the practice’s own fault — they didn’t realize the magnitude and the commitment that was going to be necessary to be successful. Sometimes they just have buyer’s remorse, but it’s a good product, it works fine. But the practice didn’t realize that there was going to be a pretty big commitment.
Then, the second thing that’s probably just as common is a lot of times they just flat out bought a defective product or something that was not going to work at the point of care. It looked good in the demo; the vendor made a lot of promises. But at the end, it started to not perform as promised or as expected. Then people get discouraged and frustrated.
I would say the third mistake is contractually. A lot of those two things I just described could really be avoided if people would take the extra time to create a statement of work, or to develop terms and conditions tied to the goals and objectives of the project. Everybody’s aligned around the same outcome, so you can set up your payments with the vendor to be tied to outcomes.
I always compared it to building a house. You would never pay the roofer before you pay the foundation guy. You do it based on stages and phases. With each phase being successfully completed, you move onto the next phase and you structure your contract based around successful completion. You have a lot of testing, and build and validation built in to that, so that way you’re not just kind of going on blind faith alone.
Do any vendors come to mind in the ambulatory care space that you think are consistently doing things right in terms of product, implementation, and support?
The KLAS surveys tend to track that around customer service. I look at vendors like Allscripts that have unbelievable market savvy, but they have five EMR systems and four practice management systems. At the point of sale they’re talking about a MyWay product, a professional product, an Enterprise product. I think that’s what the hard lesson is. We’ll look back in five years and what they’ll ultimately do is commercially discontinue a lot of those products.
While I think they’re doing a good job selling it, I don’t know if it’s in the market’s best interest to have one vendor throwing multiple products into their stable because it doesn’t serve the vendor very well and it doesn’t serve their customers very well. I tend to think vendors that are very exclusively committed to a single product strategy — like an Epic, like a NextGen, like a Greenway — are ultimately going to come out better.
You look at vendors like, even GE, Allscripts — they get weighted down big time with having that many variations of their product. If you look at the legacy vendors — IDX, Misys, Medical Manager, all of which threw out multiple versions of their products because it allowed them to generate multiple levels of support arrangements — at some point in time, that’s just not sustainable, and it’s probably going to be even more difficult to sustain it as requirements for product certification get more stringent. Now they’re going to have to decide who they’re going to cut and who they’re going to keep because it just isn’t practical for these companies to maintain that many overlapping products.
So, the ones doing it better are the companies that have chosen a niche and are sticking with it, as opposed to trying to reach every end of the market?
I would say companies that are committed to a true, fully-integrated, single enterprise solution, versus ones that cobble a bunch of things together. On the low end you have the e-MDs and the eClinicalWorks and the Greenways. In the mid-range you have the NextGens. Allscripts is probably there if you want to segment them towards just a couple of their products.
I don’t think anybody believes the old Misys application’s going to stick around. In fact, they’ve already started sending out letters to upgrade or move over those people. Epic certainly is a clear, good example of a vendor who’s totally committed to their own development, their own product. They have a lot more control over how the product works and performs, and they’re not always relying on third-party cobbled systems together.
Do you think HIMSS includes a good representation of ambulatory providers and vendors?
They didn’t always, but they are now. I think that has been their biggest area of improvement is that they have finally started to reach out to ambulatory. I’m seeing where before, only my hospital clients even knew about HIMSS, and now I’m starting to find that the ambulatory people that we’re working with are attending it and becoming members of HIMSS. I’ve actually seen HIMSS making an effort and trying to reach out into ambulatory.
I also think that that aggressive effort was one of the reasons why TEPR was unsuccessful, because HIMSS, about three years ago, started going after that market and there just wasn’t room for two of them. TEPR did really reinvest a lot of it back into driving attendance, where I think HIMSS, at least they get good attendance. There will probably be a point in time, I don’t know exactly when, where HIMSS may become just a conference to network with your existing customers because of all the selected systems — or until the next thing that re-emerges. But I do think they are really making good strides and progress in reaching out to the ambulatory side.
Do you think that one day they could be a threat to, say MGMA?
You know, it’s funny. MGMA didn’t initially have a lot of IT presence until EMR became popular. Five years ago, if you went to an MGMA conference you found CTAs and billing companies and professional service-type companies exhibiting, but very few vendors. Also, MGMA is almost usually attended by office managers and by administrative.
I’ll give you an example of how trade shows evolved. AMGA, which is similar to MGMA but it’s exclusively focused on large, multi-specialty group practices — they just had their annual conference in New Orleans. I’d say 20-30% of their members are Epic customers and Epic didn’t even have a booth there, but Judy was walking around the floor and meeting her clients. She says, “Hey, I come here to see my clients.”
Very few vendors were exhibiting and the reason why is if you look within that membership and that trade association membership, 90% of those members already have an EMR system. So the few vendors that were exhibiting, they were exhibiting extra modules like patient kiosks, Web portals. They were there to try to sell additional services to their customers. But I think MGMA is going to always have a market because they’re appealing to the smaller primary care ambulatory space; whereas, HIMSS is 100% focused on healthcare information technology and the MGMA covers a much broader range of topics.
What’s your prediction for the physician EHR adoption three years from now?
I think in spite of the stimulus money and whatnot, I think it’s very unrealistic that we can get this many physicians through the system in this short period of time. One prediction I do have is that there will likely be an extension of the stimulus. I do think Obama wants to spend the money and he’ll make it easy. I mean, the bar’s been set kind of low as it is, but I do think that there will be an extension of the deadline so we have more time for more people to get through it.
My fear is that if there is this massive rush, I think that we run the risk of doctors getting first, bitten by a bad experience — which could actually cause us to backslide a little bit. I also think that if there’s a massive rush, then a large percentage of our doctors trying to do this are going to buy systems from “two guys in a truck” EMR company and in three years, we’re going to have to recycle a lot of those people back through because that vendor couldn’t hang with the requirements as they get more difficult each year.
I do think the market’s going to continue to compress. There’s going to be more vendor consolidation and the market won’t have as many players in it, which means that a lot of the early adopters will have to recycle back through.
What percentage adoption do you think will be in say, 2013?
We tried our best to get the exact adoption rates because you know adoption rates have been all over the map, anywhere between 4 and 40%.
The CDC did a study and they concluded that 40% had EHR. Well, it depends on how you ask the question, so they went back and re-surveyed. They said, “Of all you folks that said you have an EHR, how many actually have a certified system, one that meets Meaningful Use requirements as we know it today? Actually uses the system at the point-of-care and has it integrated?” Let me ask the question that way — only 4% said, “Well, if that’s what you’re describing an EHR as, then that’s what I have.” There’s a slag between what people think they have, versus what they really have.
We tried to sort of prove it out ourselves, so we went to the AMA to find out exactly how many physicians there were. We took out all those that worked in academia. We took out those who were physicians, but worked in a hospital, like a radiologist, an anesthesiologist, those that couldn’t really buy an EMR. We took out those who worked in corporate medicine — they’re doctors, but they weren’t practicing. That left us with about 600,000-700,000 physicians who could even buy an EMR if they wanted to. So we said, “OK, well this is real easy now. Now that we know how many people can actually buy one, all we’ve got to do now is go ask the vendors how many systems were actually sold.” We contacted every vendor that we possibly could, and by the time we contacted about 60 of them, the vendors had somehow managed to sell more EMR systems than there were physicians to buy them.
I’m not surprised.
What happens is when you try to get market share from the vendors, they continue to count systems that have been sold, but they don’t ever really go back and count systems actually used. That’s the problem with our reporting. All vendors are counting systems sold, but not actually implemented. I would say that if the vendors were totally honest, 20-25% of systems sold never get implemented. They just stop using it for whatever reason or they change to something else and the vendor doesn’t reconcile their user count because they’re basing it on X number of licenses sold over their years of business. Also, a lot of vendors double count.
Allscripts, I love their statement: “One in every three physicians use Allscripts.” Really? When you unpack that, you may have somebody that’s on an old Medic Plus system that’s been discontinued five years ago. You may have someone using PayerPath; you may have someone using the handheld e-prescribing tool that they have.
But I do think adoption is going to continue to climb. I personally believe that true adoption — using an EMR at the point of care; a real EMR at the point-of-care, not a “lite” or transcription — is probably somewhere between 7-10%. I think in that time period we’ll probably see it move up to 15-20%. I think it also depends on the carrot and the stick. If the stick gets bigger, which it probably will, then we’ll probably see that move a little faster and a little higher.
Any other thoughts or comments you’d like to share?
I enjoy HIStalk. It’s always an honor and a privilege to be asked to contribute. You guys do good work. I’d be happy to do it again in the future.

















The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…