Joel A. Feinman, PhD is a psychologist and Board Chair, President and Associate Medical Director for Valley Medical Group, Greenfield, MA.

Give me some background on your practice.
We’re a primary care practice – multispecialty. We have four centers. We have about 60,000 patient charts; about 60 providers; about 350 staff; in western Massachusetts.
What kind of technology are you using in the practice, in terms of your electronic medical records and billing software?
We’ve been an athenahealth practice since the end of 2000, using their practice management system. Then we brought up athenaClinicals one year ago, so we’re totally integrated on athena right now.
Are all your physicians actively using the EMR piece of it?
All of our primary care and MDs are using it. The only folks who are currently not using it routinely are our optometrists and our behavioral health therapists. But, all of our MDs are using it, all of our PAs, NPs. Our psychiatrists use it to prescribe and order, and get lab results. The subspecialties, such as rheumatology, podiatry, endocrinology, are all using it as well. The other thing we should say is we have our own physician’s office lab, and so the laboratory’s up. We have our own in-house radiology systems, so our radiologists use it as well. Although, for radiology, they’re using an athena interface at the moment; it’s not directly integrated.
And your lab is integrated?
We have a results interface, but the orders are not interfaced, and the lab information system is LabDAQ. It’s not integrated on the order side, but it is on the results side. The important part is that whenever one of our physicians orders a lab, there’s a process to get their lab into the EMR, and then into the lab information system. Then the result comes back to their inbox in the EMR. That part is solid.
Usually, when practices are moving to EMR, the biggest problem tends to be change management – changing the behavior of the clinicians. How did you overcome that?
We did this in several phases because this is our second EMR. We had a previous EMR that we were basically a beta customer for. We thought it was further along than it was. So, we went from paper records to this previous EMR, and a lot of the sweat and strain, I think we kind of got it over with in that transition. But, you never get over all of it.
We got people used to using the devices that they’re using. We got people used to figuring out, “What’s the stuff I really need to see in the EMR?” We got people just used to the idea of using this kind of technology. That system didn’t work well, so after about a year and a half, we began to search for the next system.
By then, athenaClinicals had matured quite a bit and we decided it would be better to have a totally integrated system than one that would have an EMR integrating with our practice management system, via interfaces. So, the change management really was about the first system.
I think the change from the first system to athena was fairly easy because, number one: people were used to the devices. They were used to having an electronic system, and they were searching for some relief from the system that didn’t work well. We brought everybody up, I think, within a week. The first EMR, we brought people up in stages – one health center at a time. Whereas, when we went to the new EMR, the athenaclinicals product, we had to bring everybody up at the same time. It went very smoothly compared to our first time around.
I understand that Valley Medical was recently certified as a medical home. Tell me a bit about that qualification process.
We belong to a physician practice organization from one of the local hospital’s groups. They came out and they did a practice assessment for us where they went through all the different standards and elements that are required for the NCQA certification for medical homes, and they actually rated us – how we would rate against the standard.
After that practice assessment was completed and we got our results, we realized that a lot of the processes and procedures and policies that NCQA was looking for were already in place, in terms of Patient-Centered Medical Homes standards. It was a no-brainer for us then, to move forward and actually become certified, and actually apply to be certified and review our records and commit.
After we finished the practice assessment, then, of course, there were areas that were highlighted that we needed to either tweak the policy, or make slight changes. Or, maybe even create a new process that we hadn’t thought about it. So we went through a six-month period of looking at how we deliver care to patients and what areas we needed to improve upon – writing new policies, rolling it out to the staff, re-measuring and making sure that the new process was incorporated into the daily workflow of our staff.
Then, after that was completed we did some mock chart reviews just to see how we would measure up against the standards for the chart reading portion. Again, we did pretty well in that. It highlighted some areas that we needed to improve on as far as how we document. Not that we weren’t providing the care, but we needed to improve how we’re documenting it in their medical record.
One of the major areas that we found that we didn’t do well was documenting progress towards patient goals. We didn’t have goals for the patients. We weren’t good about saying, “We want you to reach this goal, and this is how we’re going to help you do it.” So, we had to go back to the physicians and the practitioners and the clinical staff, and everybody worked together to document what was necessary. We did that for about three months, I would say. We re-measured and kept looking and seeing how people were doing with the changes. Then, we actually set our survey date.
In the meantime, we were compiling all these documents and putting them in a folder, like an electronic folder that would be submitted as part of our certification process. Then we had a chart review, and that took three days. It was a pretty intensive chart review. It was basically 36 charts for each medical provider – MD provider – in our primary care practice. The charts had to be of patients that were seen for our three clinically important conditions. What they mean by clinically important conditions is usually the conditions that you see the most patients for, or are the most chronic in your population, or would have the most benefit of being managed better.
Our three clinically important conditions were diabetes, hypertension, and coronary artery disease. After we compiled all the chart review results, the whole package got submitted to NCQA and it was about a 30-40 day waiting period before we found out if we had passed. We passed with flying colors.
You mentioned in here that there was a lot of information that you had to compile along the way. How did the EMR facilitate that?
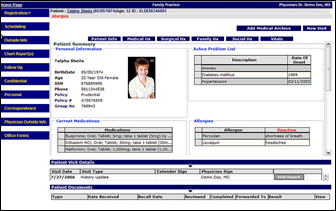
The EMR facilitated that because it was very easy to go in and take screenshots of different areas of the electronic medical record. If we needed to show that we manage our patients who have a different language, we could go in and take a screenshot of the actual field in the EMR that document the patient speaks Spanish, or that the patient needs an interpreter.
Do you think that if a practice did not have an EMR it would be possible, or challenging to do a qualification?
I think it would be very challenging. I don’t think you actually have to have electronic systems, but I can’t see how anybody would pull that off without one. It would be very time consuming and very difficult. Even more important than meeting the qualifications for NCQA, I can’t see how you could have a Patient-Centered Medical Home without some way of aggregating information, making it available to point-of-care and updating it constantly; having it available whether you’re in one building or another, having a medication list that’s accurate and up-to-date and readable; having a problem list that is accurate, up-to-date, and readable.
So the issue of getting yourself certified, I think, would be very hard to do that on a paper system. But the more important issue is how you take care of patients. I don’t see how you can do that anymore without some kind of electronic system that actually works.
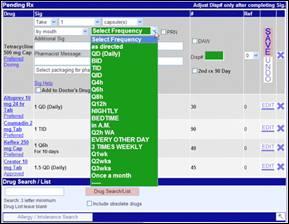
The other thing the EMR affords you is that you can template things so that you know that the important parts of the documentation aren’t going to be missed. When you have a piece of paper, you can write anything on a piece of paper. But if you have an actual templated visit for say, diabetes, that goes through X, Y, and Z of what needs to be covered at that visit, it prompts the provider to make sure that they cover all the bases.
I assume that you’re also going to be trying to qualify for the ARRA stimulus money?
Yes.
How has your use of the EMR changed now that we have a clearer idea of what the Meaningful Use requirements are going to be?
I don’t think it’s changed at all. I think that the product itself was designed, set up, and actually works, in a way that will meet the Meaningful Use criteria – maybe with a couple of tweaks here and there. We haven’t changed the way we’re using it, but we did just bring up our patient portal. I think that is one way that we’re going to hit a homerun with Meaningful Use.
That’s just one of the things that’s so useful for us about athena is they’re busy scanning the federal regulations to make sure that their product is going to meet this criteria. For example, the patient summary, we always were able to provide the patients a summary of their visit, but the system has now been configured so that it’s really easy to track that we’ve given that information to the patient. So yes, we’re sort of catering to that Meaningful Use, but mostly we’re just using the EMR to take care of our patients.
Even with all these opportunities for stimulus funding and whatnot, there are still many physicians who are avoiding adopting EMR. What do you think needs to change in the industry to increase physician adoption?
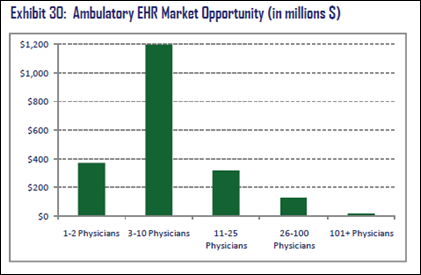
For the smaller practices, I think even the stimulus money itself probably doesn’t get a doctor or a doctor’s practice to the point of saying, “I absolutely have to do this, or else.” There’s a lot more money that physicians will have to spend to get EMRs up and running than will be reimbursed by stimulus dollars. I think most practices are realizing that you simply cannot manage in a paper world anymore. If they haven’t hit that reality yet, they’re going to hit it soon. I think that’s going to drive them as much as the stimulus dollars, to some electronic system.
Plus, I’m really hoping that we get to the point in the healthcare system where there is some kind of master plan that allows sharing of information easily and accurately, and securely. So if my mom’s in the hospital in Florida, and her doctor is in Massachusetts, that ER can pull up her med list.
When I’ve talked to small physician practices, what they tell me is they’re waiting to know what the data exchange is going to look like, what information has to be kept. Everybody’s afraid of signing up with an EMR that’s going to disappear or not going to meet Meaningful Use, or not going to be able to be used in any of these regional information exchanges. I mean, it’s like all the people that invested in the Betamax video players, and then they went away because the VCR ones took over. People are afraid to invest in the Beta.
In Massachusetts, for instance, there’s already legislation that’s mandating physicians have some electronic system by 2013. I think the handwriting, clearly, is on the wall; I think a lot of the stuff is what you talked about before about change management. It’s a money issue. There’s the “assure me that this is really good for my patients and I’m going to have some real benefits from this.” Then, there’s “Oh my god, how do I actually make this happen?” That’s a big hurdle.
But, the more practices start doing it, the more other physicians are looking around at their colleagues and saying they need to get on the bandwagon.
Have we reached the tipping point yet, or is that still to come?
Well around here, I think we’re close to the tipping point. There are still a lot of practices that haven’t made the plunge yet, but they’re getting very serious, so I think it is coming. The other thing is people are probably getting tired of being badgered by the 50-60-70 companies out there – advertising and calling them, and sending them emails. At some point, that herd is thinned out to 5 or 10.
Practices will be fine as long as they’ve done enough homework and confident that the one they’re buying is going to be around for the long haul. I think we’re pretty convinced that the one we have is going to be around for the long haul.















The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…