HIStalk Practice Interviews Albert Santalo, CEO, CareCloud
Albert Santalo is chairman, president, and CEO of CareCloud of Miami, FL.
Give me some idea about the size of the company, number of employees, revenue, and the number of practices live.
The company is about 120 employees now. We’re managing around $700 million in accounts receivable for clients. We don’t disclose specific revenue numbers, but we’ll be in the $10 million or so range for 2012, anywhere from $8 million to $12 million.
How many practices do you have live?
The number of practices is probably 250 or so. They range in size from solo practitioner to larger, multi-specialty groups. It’s well over 1,000 providers.
Countless companies offer PM and EMR systems and several of those have cloud-based solutions. What’s your competitive differentiator and what companies do you see as your primary competition?
We see lots and lots of companies, and we group them into different categories. Almost every company that’s out there that has had any type of success has started in practice management or medical records and bought another company with the other discipline. Very, very few have built what I would call an industrial strength solution for both sides from the ground up on a common architecture.
When you think about the way a medical practice works, the clinical side is not really separate from the financial and administrative side. The whole thing starts with an appointment. At some point, there’s a handoff to a clinician who uses a medical record system. Then it goes back into the billing process to get the doctor paid for what they do. There’s too many clunky handoffs between these old, fragmented systems.
Most companies just haven’t gone to the trouble to build this all on a common architecture. I would say it’s a subtle differentiator for us because most people don’t really get it. But the reality is that when you look at our system and you see what kind of elegant, beautiful experience it is from cradle to grave, it becomes obvious that this all should be built on a common platform.
Yes, there are a few cloud-based players, but most of them built their systems in the late ‘90s or early 2000s. The Internet-based tools to build these systems have evolved two or three generations later, and that is what we’re using.
For instance, some of our competition only works on Internet Explorer on a Windows PC, while the world has changed in the last few years. A lot of physicians are using Macs — if not at work, in their personal lives. There are mobile devices, and physicians need to be able to access information anywhere. A lot of people don’t like Internet Explorer — they want to use Google Chrome or Firefox or Safari. We built this the way you would build it in the last few years, which is so that it works ubiquitously on any browser.
What companies would you say are your primary competition?
We come across all sorts of existing solutions. We compete with traditional players such as Allscripts, Greenway, NextGen, etc. But at the end of the day, the only company that we really feel sees the world the way we do and has built something like what we are hoping to achieve is athenahealth.
You allude to CareCloud’s slick user interface. Does the user interface offer a sustainable advantage given that these entrenched companies theoretically could freshen up their user interface to resemble yours?
That is an issue, but what I would ask is has anyone really been able to duplicate Apple’s user experience? It’s not like it’s not there and everyone can’t use it. Yet all of the stodgy, old companies struggle to create a user experience like what Apple has created.
One of the things you have to understand about CareCloud is that design is ingrained in our DNA. The first person that I hired when I founded the company was Mike Cuesta, who comes from a graphic design background. In other words, Employee #1 was a designer.
It’s really hard, especially when you’re a bigger company, to get design woven into your culture if it wasn’t already there. Design isn’t something that’s done by consensus. Bigger companies tend to be a little more democratic, for lack of a better word, and committees don’t design well. Design is done by really, really talented designers.
On top of that, some of the technologies that the competition uses are not easily employed in a design type of a way.For instance, if you look at somebody who’s developed in straight-up HTML, you know they have to make the leap to HTML5 to really do rich Internet applications, and the HTML5 development tool kits are not there yet. It’s easier said than done, but the reality is as people are imitating our current designs, we’re already working on the next generation of something even better.
Do you have a sales force?
We do. We’re selling the product through a combination of a traditional sales force and through online marketing. As of late, we’ve been ramping up the sales force pretty significantly. I’m amazed at the amount of people defecting from the old world to come here and deal with something new. I’ve been shocked at the talent that’s been showing up, and we’re hiring them.
We’ve got eight new sales people showing up here Monday for training. That will be the next wave, and there’s a wave after that.
Geographically, they’re located all over?
Throughout the US, everywhere from the northeast to the West Coast.
Any plans to distribute the product through resellers?
Yes. There’s a lot of traditional VARs and such that are out there, and especially with larger installs, we can use help with implementations. In fact, we’re already working with some VARs that are partnering with us to put our solution into their client base.
You recently launched CareCloud Charts. What are the advantages and disadvantages of entering the EMR market late in the game, especially late in the ARRA game?
We could have entered a lot earlier, but we’re big believers that we just have to build things correctly and not rush them too much. You have to always build on a strong foundation.
I would say that the disadvantages are that there have been a lot of people that have purchased the EMR already, but there are also a lot of people that have gotten burned in that process. They’ve been chasing the Meaningful Use dollars and they realize that they made a poor choice in what their EMRs are.
The good news is that they already have bought into the EMR as something they have to do, but a lot of them are looking to swap it out. We’re seeing a lot of that. With our type of solution, which is really pay-as-you-go, it’s a pretty easy transition from a financial perspective, because they don’t have to buy eight servers and do all sorts of creative stuff like with other solutions.
The other about coming late in the game, something that isn’t quite apparent to everybody yet, is most of the EMRs — if not all of the EMRs that have been written and developed up until now — have been developed with the idea that what we’re trying to do is capture the information as it relates to a doctor and a patient seeing each other in a brick-and-mortar type of setting.
The reality is that the world is moving towards much more of a real-time, instrument type of model. We envision that in the not too distant future, people will be wearing sensors. They’ll be stepping on their scale in their home, and that scale will be connected to the Internet, taking their blood pressure, etc.
The way we’ve designed our clinical system is such that it lends itself to this real-time world, where there’s lots and lots of data being captured in real time on specific patients. The system has to provide strong analytics and alerting to the providers so that they’re not inundated with all these data.
It’s a very, very different architecture than what’s out there, especially if you compare it to systems that are written in MUMPS, which is technology from the ‘70s. As you know, this is what you see in healthcare IT. It’s ridiculous. We wouldn’t buy any piece of technology in our personal lives that had anything in it from 1967, yet people are spending tens, hundreds of millions of dollars on systems like Epic, which is crazy.
You’ve said that CareCloud offers a social infrastructure. Explain that.
Think of the social infrastructure like this. When you really look at healthcare, it is a social business. Today, especially with the kind of the fragmented world that we live in on the provider side, a patient bounces around from practice to practice as they’re getting care. A primary care doctor may refer a patient to a cardiologist or urologist, but there isn’t any good infrastructure to push data between these providers.
People talk about HIEs and things like that, but the reality is penetration of HIEs is very low. We’ve built a secure, social framework within our system so that that data is usually pushed from person to person, business to business so that it’s not captured again. It doesn’t infringe on the patient experience, so that errors aren’t introduced. It really speeds up the delivery of care and can help eliminate some of the redundant care that exists.
We think of an HIE as, “Why can’t an HIE be a secure Facebook as opposed to this thing where I have to get my CIO to talk to your CIO?” Guess what? Most doctors don’t even have a CIO. This whole integration between practices and systems is not realistic in ambulatory healthcare. We built it as a friendly place where everyone can interact.
If I use eClinicalWorks or athenahealth, I can access the social infrastructure?
Yes. We’re not there yet in terms of those capabilities, but yes, you will be able to access that infrastructure. Absolutely. And our hope is that you’ll stop using eClinicalWorks. [laughs].
In your various company announcements, you talked a lot about investors, innovation, and awards. You don’t say a lot about customer successes. Who are your notable customers and what have they accomplished using your product?
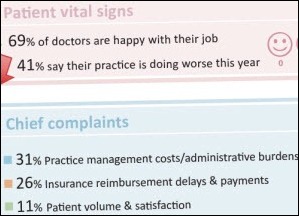
There are many, many flavors of customers that we have. Some are larger, some are smaller. The successes mostly relate to financial successes. That’s the biggest way that we measure the success around here, that these practices are able to derive more revenue from what they do. Because, as you know, a lot of practices do a lot of work and don’t get paid properly for it.
That’s the first piece, and at the same time, they are able to save on a lot of costs because we convert what’s typically a fixed cost to a variable cost. There are so many bills and this is thrown into our offering that they just do it a lot more effectively and more cheaply.
Your EHR product has been ONC-certified, correct?
Yes.
Have any of your early users been able to attest?
They need to use it meaningfully for 90 days. We’re not there yet, but that’s coming.
As you know, there’s a lot of noise in the system around this whole thing. Although you spoke of the timing earlier, we’re still early in the game in terms of the attestations. You can even see the people that are making a lot of noise, like Practice Fusion. They say they have 100,000-something providers. They only have like 100-and-something providers that have gotten Meaningful Use dollars, which is abysmal, in my opinion.
Any additional thoughts that you’d like to share?
We’re very excited about what’s coming this year. There’s a lot of innovation we’re going to be releasing. We worked very hard in making sure that the EMR was ready for the marketplace, but now, a lot of what happens now that the product is completely rounded out, is a lot of building on top of what we already have. It will be a tremendous amount of refinement. There will be a movement into the mobile space and so forth this year, so it should be pretty exciting.










Re: Walmart Health: Just had a great dental visit this morning, which was preceded by helpful reminders from Epic, and…