Over time the use of open notes will become the standard of care, predicts that the authors of a NEJM-published op-ed. The clinician-authors note that increasing patient engagement through transparent medical records contributes to improvements in health, care, and costs, and that patients who access their notes have better recall and understanding of their care plans and better medication adherence.
E-MDs Cloud Solutions v. Cirrus achieves ONC-ACB certification for MU Stage 1 and 2 and is compliant as a Complete EHR 2014.
Deloitte includes Kareo on its Technology Fast 500 list of fastest growing technology, media, telecommunications, life sciences, and clean technology companies in North America based on its 797 percent growth over the last five years. Kareo was ranked fifth in HIT and 156th overall.
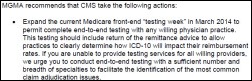
Troubling: the healthcare industry is making slow progress on preparing for ICD-10, according to a WEDI readiness survey. About 20 percent of vendors claim they are halfway or less complete with product development, while about half of providers have yet not completed an impact assessment. Meanwhile, about one-third of health plans have not initiated internal testing; two-thirds have not started external testing.
Projected physician shortages can be substantially reduced by using new models of primary care, such as the PCMH and nurse-managed health center (NMHC) models, even without increases in the number of physicians, according to a RAND study. RAND projects that if the prevalence of PCMHs increases from 15 to 45 percent and NMHCs from .05 percent to 5 percent, physician shortages could be cut in half by 2025; researchers also believe that medical homes could handle 20 percent more patients through the use of technology and improved coordination.
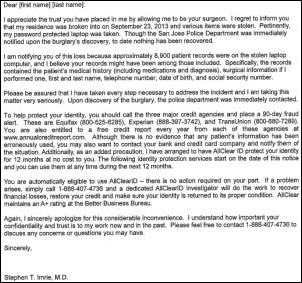
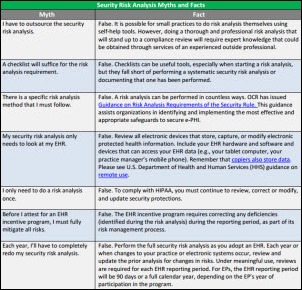
Solo physician Stephen T. Imrie, MD handles a potential data breach in an arguably more efficient manner than many larger organizations with presumably more resources and available expertise. The San Jose-based physician sent an appropriately apologetic letter to 8,900 patients notifying them that a password-protected laptop was stolen from his home September 23. The computer included both clinical and financial details on patients, including patient social security numbers. Though no misuse of data has been reported, Imrie automatically signed up his patients for free credit monitoring.
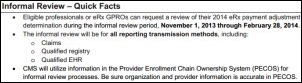
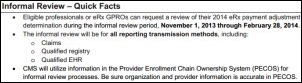
CMS implements an informal review process for EPs and group practices who will be subject to the 2014 eRx payment adjustment. EPs/group practices have until February 28, 2014 to email eRxInformationReview@cmg.hhs.gov to request an informal review.

A big welcome to Optum, HIStalk Practice’s newest Platinum sponsor! Optum, which includes the OptumHealth, OptumInsight, and OptumRx divisions, offers a wide variety of products, tools, and services for various segments of the healthcare system. Their technology offerings for hospitals, physicians, and other stakeholders focus on the delivery of integrated, intelligent solutions for modernizing the healthcare system and improving health. Solutions for physician practices include Optum Claims Manager and Optum Intelligent EDI, which are designed to help practices submit clean claims the first time around and maximize reimbursements. Claims Manager can be directly integrated with third-party clearinghouses, billing systems, and PM systems, as well as with Intelligent EDI, Optum’s claims processing solution that successfully provides first-pass payment rates as high as 97.5 percent. Optum also sponsors HIStalk at the Platinum level and we thank them for supporting of our work.

Greenway Medical adds Digital Assent, a provider of patient satisfaction survey solutions, to its online Marketplace of value-added partners.
If you are a physician and looking for some moonlighting ideas to pay off those holiday bills, here are a few suggestions from Medscape. Options include telehealth consults (pays about $20 for a 10 minute consult); health insurance claims reviewer ($85-$200 an hour); and, cruise ship doctor ($150 a day plus free cruising for you and a guest.) Can’t imagine why anyone would choose to review insurance claims over a free cruise.

Email Inga.











The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…