News 8/15/13
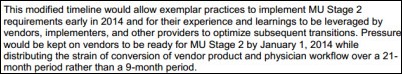
The AAFP urges CMS to modify the Stage 2 MU timeline because of concerns that the program’s requirements will “outstrip the capacity of many certified electronic health technology vendors and ambulatory family medicine practices.” The AAFP offers a proposal that does not delay the implementation of Stage 2 but adds a 12 month extension to the timeframe for Stage 2 compliance.
MGMA-ACMPE announces that HCA Physician Services, which employs more than 500 practice managers, is the association’s newest large group member.
Aprima reports having over 600 participants at annual user group conference earlier this month in Dallas.
Greenway Medical joins Humana’s EHR Rewards program, which subsidizes 85 percent of the purchase of select EHRs for physicians practicing in the Humana network.
Frost & Sullivan awards Kareo its 2013 North American Physician Practice Management Customer Value Enhancement Award for demonstrating excellence in implementing strategies that create value for its customers.
Mercy Health System (ME) selects Allscripts RCM Services for its physician practices.
Bogdan Rau of the UCLA Center for Health Policy Research creates an interesting table depicting the top EHR vendors based on the percentage of MU attestations. While Epic and Allscripts have dominated the top spots since 2011, it’s interesting to see how the vendor mix has shifted for the vendors in the 3rd, 4th, and 5th place spots. Obviously the number users by vendor has a big impact on the rankings.
Email Inga.



















The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…