News 7/30/13
Zotec Partners signs a definitive agreement to acquire Medical Management Professionals , a subsidiary of CBIZ, for $200 million, making the new entity one of the largest RCM services firms in the US.
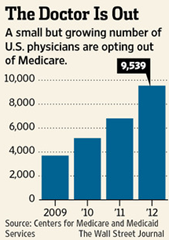
CMS reports that the number of physicians opting out of Medicare has tripled since 2009 because of low reimbursements, displeasure with the government’s involvement in medicine, and patient privacy concerns. Despite the growing trend, the overall number of physicians who had previously accepted Medicare and opted out in 2012 is relatively small at 9,539. AAFP claims the number of family doctors accepting Medicare patients last year was 81 percent, down from 83 percent in 2010.
The California Academy of Family Physicians will provide its members with tools and transformation expertise from Arcadia Solutions to help practices migrate to a PCMH model.
In case you missed it, over the weekend Dr. Gregg shared the story of a blogosphere encounter with another physician whose group recently went live on EMR. Dr. Gregg relayed this anecdote about the other physician’s implementation:
That day – go-live Day One – with no schedule adaptations, the partners were also up and running, most having documented all of their first day’s encounters on the system. Not just one or two patients, but all of them.
I asked Dr. Gregg to give me his opinion on why the practice was so successful so quickly. He points to the software (ElationEMR), which Dr. Gregg tells me is “probably more intuitive than any system I’ve seen.” He notes it does have a few “holes” but it’s only $149/month with no up front fees. I’d never heard of the software but always find it fun to learn about new programs that seemingly live up to their hype. Dr. Gregg and I have no financial interest, by the way. Just the regular ole nerdy interest.
ONC head Farzad Mostashari, MD and MGMA Healthcare Consulting Group’s Rosemarie Nelson will provide keynote addresses at this week’s Aprima 2013 Annual User Conference in Dallas. On August 3, attendees will make fleece blankets for ICU patients at The Children’s Medical Center of Dallas.
CareCloud reports it signed 150 new medical groups in the second quarter, with more than half selecting CareCloud’s integrated EHR/PM applications.
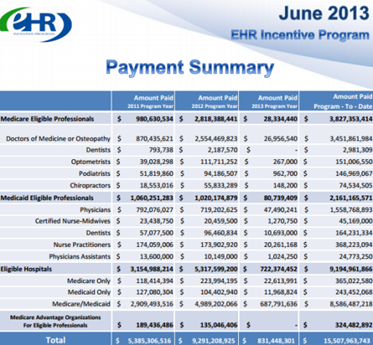
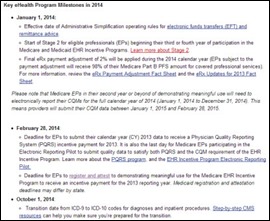
Though the end of June, 305,778 EPs have been paid more than $595 million in EHR MU incentives.
Walgreens announces a rebranding of its 370 retail clinics, including a name change from “Take Care Care Clinic” to “Healthcare Clinic.” I bet Walgreens paid millions to advertising gurus to come up with that catchy name.
















The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…