From the Consultant’s Corner 1/1/13
The Election is Over. Now What?
With the reelection of President Obama following on the heels of last summer’s Supreme Court decision, it’s clear to me that the Affordable Care Act (ACA) and all its ramifications are here to stay. In my opinion, physician practices can no longer delay; they must figure out how to successfully navigate the numerous changes coming to healthcare.
For one thing, reimbursement levels will continue to decline. As politicians hash out how the country will avoid the “fiscal cliff”—a collection of drastic tax increases and spending cuts slated for January 2013— I think the topic of cutting Medicare and Medicaid funding is sure to come up. And history tells us that when public programs reduce reimbursement, private payers follow suit.
In addition, the whole manner in which physician practices get paid is changing. In chatting with many of my clients, I can see that the fee-for-service reimbursement model is quickly fading as outcomes-based programs, such as pay-for-performance, value-based reimbursement, accountable care, and the like gain more popularity. With these new models, I think small practices will be forced to take on more risk and assume responsibility for larger patient populations. This will certainly be challenging, and many practices will seek partnerships with other practices or hospitals to become part of a larger entity that’s better able to absorb increased risk.
I also believe that patient access is going to be an issue to contend with, as the number of patients with insurance increases. Patients will have more choice as to where they want to receive their medical care, which I believe will drive up competition. Small practices will need to expand access and gear up marketing efforts to hold on to their current patients, and perhaps seek out new markets in which to grow the business.
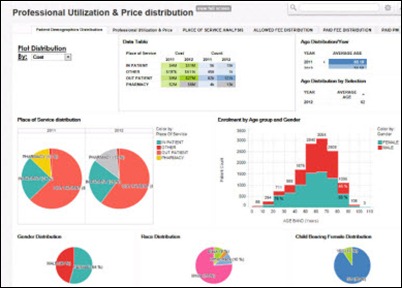
One common element associated with all of these coming trends is the need for accurate and comprehensive data. For example, in order to receive full reimbursement, I think practices will need detailed information to demonstrate the quality of care they provide. If I ran a practice, I would also want to leverage data to identify areas where cost reductions and efficiencies could be gained—not to mention enhancements to patient care.
To ensure data availability, I have noticed many practices already starting to eye their current IT systems to see whether they’re able to support the necessary information sharing and transparency for the post-ACA world. A lot of my clients are starting to shift their focus from having multiple “best in breed” systems that handle different aspects of the practice (e.g., medical records, billing, practice management) to having an integrated IT platform.
At the end of the day, I think practices need to take a strategic approach to IT selection and look beyond just the costs of a system, examining how the technology will prepare the practice for a future that depends on data. I feel it would be wise for practices to think about how an integrated IT system might support better coding, greater efficiency, reduced liability, improved quality and enhanced safety. All these things can further reduce costs and help the practice thrive long-term.
Although the future is not certain, things are much clearer than they were before last month. If I were to make one recommendation for the coming year, I would suggest that practices start thinking strategically about how best to leverage technology to realize a successful future.
Jeff Wasserman is VP of strategy and executive leadership services for Culbert Healthcare Solutions of Woburn, MA.











The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…