News 10/4/12
From Patrick Hall: “Re: Official e-MDs response. As of Oct. 1 of this year, e-MDs is pleased to report its continuing consistent pattern of year-over-year overall revenue growth. Compared to last year, e-MDs has a greater number of customers and employees, a larger number of contractors, as well as increased revenue. As a general rule, e-MDs does not comment on individual personnel changes that occur during routine business operations.” Hall is the EVP of business development ffor eMDs and we thank him for sending us this note in response to comments posted earlier this week from Adam Wright.
From San Antonio Rose: “Re: MGMA. Here’s are a couple recommendations for you. Download the MGMA12 app to your iPhone and bring your cowboy boots.” Cowboy boots: why of course! MGMA app: sounds like a great way to figure out where I want to go when. Too bad it has been stuck on this screen for the last two hours. Maybe the download will finish by Oct. 21.
The 77-physician Optimal Radiology selects McKesson Revenue Management Solutions for billing, reporting, and collections.
The Ohio AFP and the state’s department of health pilot the PCMH Education Pilot Project, which aims to transform 50 primary care practices into PCMHs that will train medical students, primary care residents, and advanced practice nursing students. Participating medical students will receive up to $30,000 per year in scholarship funds in return for a commitment to practice at least three years in Ohio.
Seven percent of physicians plan to become cash-only or concierge practices within the next three years, which will likely exacerbate existing concerns about physician shortages and lead some patients to avoid routine check-ups and screenings.
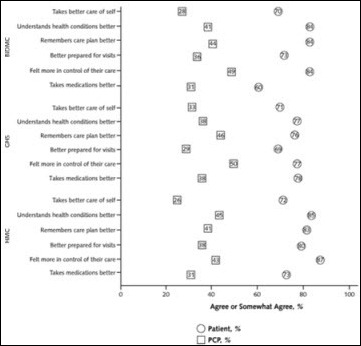
Patients who have access to their doctor’s notes are more positive about their quality of care, even though physicians are less enthusiastic a note-sharing program. A year-long study of healthcare sites using OpenNotes software found that patients are more likely to understand their health issues, recall what the doctor tells them, and take prescribed medications when they have access to their visit records. Only a third of the doctors agreed that the program changed how well patients managed their care.














The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…