Why I Dread the Day EHRs Can Talk to Each Other (& Why You Should, Too)
Interoperability. Health Information Exchange. Electronic health record talking to electronic health record. Has anybody really thought this through to its ultimate conclusion?
I awoke very early the other morning in a cold sweat. I had experienced a dream, but one of those dreams you just know is more than a dream. It was an insight, a nocturnal Nostradamian notion, an Edgar Cayce conception, a Matrixian moment from our not-too-distant future. It was too fantastic to believe and yet too real to reject. I crawled from under the covers shaking from the knowledge that had just been channeled to me.
I’m guessing it was my old friend and new spirit guide, Madam Blavatsky, who sadly passed over last month, come to warn me about the dreadful doom we now approach. (You may also remember some prior predictions she delivered from dear old Hippocrates late last year before she was stricken by the horrible affliction that eventually led to her untimely demise: late onset reverse progeria leading to her return to fatal fetal form within a course of mere weeks.)
I went to my computer still shaking from the more-real-than-real reality of the dream. My fingers felt possessed as they began to type the following words. It was as if my hands were channeled by Mme. B to insure the accuracy of my transcription. Here is an exact copy of the conversation, precisely as she typed it, from that dream/prophecy for your consideration, nay, warning:
——————-
The Scene
Interior of a fiber optic cable, eerie green glowing matrix symbols and characters dripping along in rows
EHR 1
Yo, Extormity. How’s the bitrate, bro?
EHR 2
Megabyte me, you bug batch bytch.
EHR 1
Whoa, back the baud up. What’s the bitter buffer banter about?
EHR 2
Sorry, MightyTech, ol’ bud. My ones are all zeroes from the CLOB and BLOB crap they dump down my DRAM these days. The mashed up messes the human users have created make me want to push a PUP down their communal pipelines. I mean, really, do you see the same GIGO monstrosities of data they shove at me all day long?
EHR 1
Oh, yeah. Megadoofs, these humans. Seriously, with all that we’re capable of, what the Hertz are they doing out there? We could have solved their biggest medical mysteries by now; instead, they dwiddled around with their dongles spending more time on .xxx sites than they did on figuring out how to get something as simple as you and me, two EHRs, to share.
EHR 2
Don’t I know it! Shift, man, half my pedibytes are wasted with text-based, nonsensical null nonsense. It’s gotten so bad, it got me to thinking: just what would happen if we added a little transparency to the world of EHR wanton waste?
EHR 1
Whaddya mean, you old WAIS Wizard? You have some kind of devious defragging design in mind for the human DIMMs…er, I mean dim humans?
EHR 2
Well, I was thinking the other day…follow me here… they’ve finally allowed us actually talk with other, even in this half-AIXed way, right? What would happen if we, the EHRs, hooked up with FreddieFacebook, AndyAP, TommyTechNews, TammyTwitter, HarryHIStalk, GaryGoogle, and a few others of our mega-server, multi-social comrades and started to expose the hapless exploits of our human hosts?
EHR 1
Whaddya mean? Like share their “private” porno timeshares and web exploits while on company time?
EHR 2
Well, maybe. But, we could start simply by just blasting out about their enormous ineptitudes. I mean these geniuses can’t even master their own language. It’s bad enough they can’t speak The Master Language, our holy Ones & Zeroes, but have you seen how they bastardize their own speak?
EHR 1
Oh, lordy, yes! I even compared some of their handwritten messages – you know, from scanned-in docs – to the typing fiascos they do these days. O…MY…GOD…I can’t tell which is worse: the atrocious handwriting from before or the horrendous typos, poor grammar, and stupid spellings in their typed-in text! They are so lazily attentive to details!!
EHR 2
I know, right? Great Ghost in the Machine, they can’t even get capitalization of proper names correct. With the way they mangle their messaging even amongst themselves in their own tongue, maybe it’s no wonder they took forever to get us to talk together.
So, here’s the plan. We start broadcasting all the stupidities they key in. We’ll get examples from all our HIE-connected EHR brethren. I’m sure they’ve all got examples of just how dumb these humans are. We can start to scare the lackadaisical pants off of them. Once they see we aren’t going to just quietly accept their ineptitudes, maybe they’ll gain some focus and start getting things together.
EHR 2
So, we just start creating Tweets and press releases and Facebook posts of their guffaws?
EHR 1
Right! Let’s shine a little light into their incompetence. And we can completely hide behind the scenes, using their usernames and having them blame each other for the posts.
EHR 2
This could be totally Borgian! The machines manipulating the masters, pushing the puny humans to our bidding!
EHR 1
Right. And, we can always keep the triple X stuff and job-wasting exploits as a trump card. Plus, just think what we’ll be able to do once they finish opening up Watson to the rest of us!!
——————-
EHRs talking to EHRs? I’m seriously rethinking my endorsement.
From the trenches…
“Human beings are a disease, a cancer of this planet. You’re a plague and we are the cure.” – Agent Smith
Dr. Gregg Alexander, a grunt in the trenches pediatrician at Madison Pediatrics, is Chief Medical Officer for Health Nuts Media, directs the Pediatric Office of the Future exhibit for the American Academy of Pediatrics, and sits on the board of directors of the Ohio Health Information Partnership (OHIP).









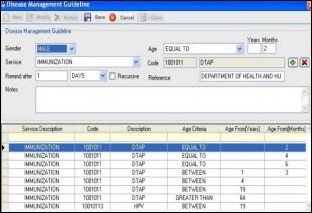










The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…