Intelligent Healthcare Information Integration 8/16/10
Help for an Amazing Pioneer
Like most of you, I try to accomplish a few things during my time here on this earthly coil. Every now and again, I start getting a little full of myself and start getting a Steve Martin The Jerk-esque “I’m somebody now” sort of feeling. You know, a “look at me, look at me” moment just like every little kid shouts to their mom or pop at some point to achieve a little validation of their worth.
Through some of what I do in the realm of HIT, and especially through some of my writing here on HIStalk Practice (thank you, again, Mr. H and Inga), I have made some pretty wonderful contacts and some even more wonderful friends. These folks come from across the gamut of healthcare, from all over the US and even from around the world. When I start thinking about how fortunate I am to have such a breadth of colleagues and acquaintances and start to consider how I’ve maybe been able to have some impact upon the growth of this fledgling industry, I can sometimes actually feel my cranium getting fuller as it begins to swell. Until…
Until I remember Sid.
Dr. Sidney Nesbitt, to be precise. Sid is a pediatrician in Nairobi, Kenya. He is one of the “blessings” I have been granted through my time in the HIT realm. He runs the Muthaiga Pediatrics Clinic located on the grounds of the Gertrude’s Children’s Hospital, a charitable trust founded over 70 years ago to help the children of East and Central Africa.
Sid’s working very hard to develop and employ advanced office design, practice management, and especially healthcare information technology techniques and tools at Muthaiga Pediatrics. His goal is to set a standard, an example that he can share with physicians all around East/Central Africa. He even engaged the interest of MIT Sloan’s Global Health Delivery “G-Lab” which worked with him for months helping him evaluate and deploy better business tools specific to the needs in Nairobi. I was lucky enough, along with the wonderful Drs. Dan Feiten of Denver and Larry Rosen of New Jersey (himself, an MIT alum) to consult with their project.
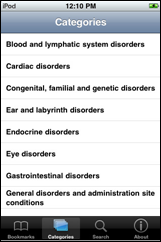
On top of this, he is the director of their pediatric endocrinology fellowship, sponsored by the World Diabetes Foundation, which brings volunteer visiting professors from Canada and the U.S. each month to help train African pediatricians. He is pioneering similar initiatives to establish fellowship programs in Africa in Infectious Diseases, Emergency Pediatrics, and Pediatric Cardiology, Gastroenterology, Neurology, and Pulmonology over the next five years.
There is more work with charitable and volunteer efforts to advance child health in Africa with which Sid is engaged than I could begin to cover here. He is planning on sharing some his amazing work this year at the American Academy of Pediatrics (AAP) National Conference and Exhibition (NCE) in October, specifically, at the “Pediatric Office of the Future” (POF) educational exhibit in a section called “Future Pediatrics International.” (I am the director of the POF, for full disclosure’s sake.)
He is truly an inspiration for me and, I’ll wager, for many, many more folks around his native Kenya. He’s a joy with whom to talk and constant source of “what others are striving to do with far less resources and far greater challenges.” He helps me remember what’s important.
But, Sid could use some help. He is springing to bring himself to America for this event, but as any pediatrician anywhere in the world will tell you, we’re not the rich boys of medicine. So, if any of you good folks out there would be able to help my friend by helping him cover just the costs of the exhibit expenses, I will do everything I can to help promote your sponsorship. Expenses cover his presentation, PC, exhibit accessories, large screen monitor rental, etc. – pricey exhibit hall fees – at the conference site, totaling around $3,000.
(FYI – The POF is doing well and getting so much love from the AAP, we’re just finishing our own web site within the NCE site – somewhat unique – which highlights, and links to, our generous sponsors. The site’s a work in progress, but you’ll see the foundation. Plus, the AAP blasts emails to some 60,000 pediatricians and has great onsite marketing providing great exposure.)
Besides the marketing potential you’ll receive, you’ll be helping one very good man. His vision and his tireless efforts to advance HIT as he seeks to help the children of Africa are those of a true pioneer.
If you can help my friend, please contact me as soon as possible here in the trenches…
“There has to be this pioneer, the individual who has the courage, the ambition to overcome the obstacles that always develop when one tries to do something worthwhile, especially when it is new and different.” – Alfred P. Sloan
Dr. Gregg Alexander, a grunt in the trenches pediatrician, directs the “Pediatric Office of the Future” exhibit for the American Academy of Pediatrics and is a member of the Professional Advisory Council for ModernMedicine.com. More of his blather…er, writings…can be found at his blog, practice web site or directly from doc@madisonpediatric.com.












The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…