News 7/6/10
Doctors continue to opt out of private practices to join health care systems. The spokesperson for Parkview Health (IN), a hospital that just picked up 11 new doctors, suggests technology assistance is one reason the hospital-owned practice model is increasingly popular. Other factors include administrative support and expertise managing the complexities of health care reform, Medicare, and Medicaid.
The California Medical Association partners with Heartland Payment Systems to offer members payment processing services, including payroll and check management.
SmartBusiness profiles Gateway EDI and CEO Charlotte A. Martin. Since she took the job in 2000, the clearinghouse has experienced 30% per year top-line revenue growth and added 200 employees. Gateway has also significantly grown the number of practices served from 5,000 five years ago to 14,000 today and acquired two companies. One of Martin’s top goals: maintaining the flexibility and intimacy of a small company.
Oregon physicians speak out against a state plan to put EMRs in place by 2015. Physicians participating in a public forum told members of a state HIT oversight committee that current EMRs are flawed and expensive and that doctors can’t afford the time to train employees and deal with software problems. I’m not sure of all the specifics in this case, but I agree that EMRs are not perfect and they cost practices time and money. However, why keep fighting the inevitable, especially when there are potential subsidies available to help make the transition more affordable? Why do so many providers keep forgetting that paper systems are also flawed and imperfect?
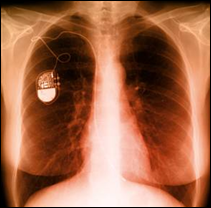
Here’s some stuff that sounds perfect for the next Michael Palmer novel. Medical experts speculate that devices such as pacemakers and infusion pumps are vulnerable to unauthorized programming and manipulation. Many medical devices use wireless connections for monitoring and programming, but those communication channels are at risk for malicious access to private information or manipulation of device functions. Maybe I have been reading too much about Russian spies of late, but the medical intrigue possibilities are fascinating, in a twisted sort of way.
ENT and Allergy Associates (NY) expands its EMR to 21 of its 31 practice sites. I surfed a bit trying to figure out what EMR these guys were running, but came up empty.
I’m hoping that HHS will announce the final Meaningful Use guidelines this week, which is traditionally one of the slowest HIT news weeks of the year. It’s the post-Independence Day lull which precedes a couple of crazy months of user conferences and related press releases on new products. I suppose I should appreciate the quiet, though in the end I am just an HIT geek looking for the latest industry scoop.
















The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…