News 2/18/14
The Colorado Health Institute analyzes the state’s looming shortage of primary care providers, which mirrors deficits across the country. The CHI offers several recommendations to address the estimated shortfall of 258 providers, including the use of emerging technology to increase patient self-care of common ailments and to advance options for self-diagnostic testing. The CHI also encourages streamlined policies to increase the use of telemedicine.
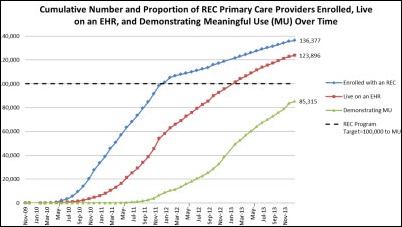
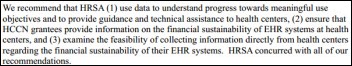
ONC reports that RECs have “far exceeded” their goal to support the adoption and use of HIT by 100,000 small practices, CHCs, and rural and public hospitals, while continuing to support providers to reach MU. I found the ONC’s announcement a little confusing since only 85,000 PCPs had met the MU milestone by the end of November, which is clearly short of the 100,000 goal.
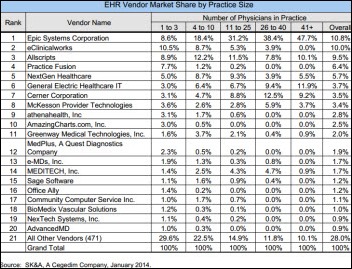
The Worcester Business Journal looks at EHR adoption in the state of Massachusetts, which is requiring all providers to sign onto the Mass HIway HIE by 2017. Small practices and certain specialized providers are most resistant to automation, largely due to cost concerns and skepticism over potential benefits. Girish Navani, CEO for the Worcester-based eClinicalWorks, notes that it will be “only a matter of time before providers everywhere will convert” to meet regulatory requirements and to recognize the benefits of sharing patient records electronically.
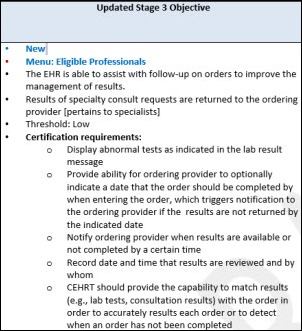
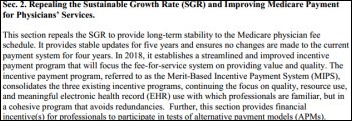
I was looking at the latest MU Workgroup Stage 3 recommendations and noted a few new items that could potentially impact EPs, should these requirements be included in the final rule. Recommendation requirements include:
- The EHR would assist with follow-up on orders, including the return of results from specialty consults to the ordering provider.
- The EHR would provide EPs with access to medication fill information from pharmacy benefit manager
- Patients would have an easy way to request an amendment to their record online to offer corrections, updates, or additions.
- Patient-generated health information could be added electronically through a questionnaire, survey, or intake form, or, through secure messaging.
The National Testing Program for ICD-10 readiness of HIPAA transactions extends certification to Greenway’s SuccessEHS solution.
Benchmark Systems will offer its customers electronic statements and online pay solutions from PatientPay. Benchmark also announces several new customers including Comprehensive Pediatrics of Brooklyn (NY) for EHR and PM, Advent Medical Group (MO) for EHR, and, Dawn’s Medical Billing (VA) and American Self (VA) for PM.
SimplifyMD version 14.0 achieves 2014 Edition Complete EHR Ambulatory ONC HIT Certification from ICSA Labs.
Researchers from the University of Pennsylvania find that dermatologists that evaluated hospitalized patients using teledermatology provided nearly identical assessments as doctors examining the conditions in person.
Email Inga.














The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…