HIStalk Practice Interviews Linda Fischer, EMR Manager, Boulder Community Hospital Physician Clinics
Linda Fischer is EMR Manager of Boulder Community Hospital Physician Clinics, Boulder, CO.
Tell me about yourself and your practice.
I have been with the hospital for almost 15 years. We’re part of Boulder Community Hospital. We have a subset that owns our practices, Boulder Community Hospital Physician Clinics. We have 17 clinics that are owned by the hospital that are multi-specialty, ranging from family practice, internal medicine, infectious disease, travel clinic, an endocrinology clinic, and we just added a trauma clinic and a neurology clinic. We also have sports medicine and occupation medicine and pain. The clinics are located within a 30 to 40 mile radius around the hospital and serve the local patients of the community.
What type of healthcare technology software do you have in place right now, and how long have they been in place?
We’re currently using Greenway for both practice management and EMR. We’ve been on it for almost four years. We converted in April of 2010. Just a couple of those clinics are not on Greenway currently. They are still using paper because they are recent acquisitions and we have not brought them up yet on Greenway. But they are in process. The hospital uses Meditech, and we do have some interfaces that run between Meditech into Greenway.
Were you involved with the selection of the Greenway system?
Yes. In fact, I implemented the legacy system that we had. And then I was part of the selection committee to bring on Greenway including the review process and then of the orientation to Greenway.
Tell me a little bit about the more recent selection process.
We had a legacy system at the existing clinics that we were on for five years. The providers did not have a choice in that system, and it interfaced directly with our hospital system. When we got a new CIO, she gave them the opportunity to stay with what we had or to do a selection process. They opted to do a selection process. So, we went through a two-year selection process where we had a number of stake holders all on the team, including IT, providers, medical assistants, front desk, and billing staff. All were on the team as stakeholders.
The main direction from IT was that the system had to be CCHIT-approved. We went through the list and people had some things that they had already researched and really wanted to look at. We grabbed about 35 of them to look at initially. We also created a list of must-haves, and then things that we would like to have. Every stakeholder put in things that the new system absolutely had to have, based on what our legacy system could already do. The dream things were things that we wished that our legacy system could do, but it doesn’t. We traded those lists, then we started to review those 35.
We looked at KLAS reviews and narrowed the list down to about ten. Did more intensive KLAS reviews and narrowed that list down to four. Then we had a vendor site fair for those four. The vendors came onsite and we had all the stakeholders as well anybody else that wanted to participate, come look at the systems that were being demonstrated, as well as maybe do a little hands-on play. We kept our legacy system as one of the four that made it that far in the selection.
What was your legacy system?
It was called LSS and it interfaced with our Meditech system that the hospital has. It was the outpatient division for Meditech and we kept that as one of the top four. Then after the vendor fair we narrowed it down to two, which did not include the legacy system.
We sent teams out to do site visits with those two systems to see how actual clinics used the systems. And, we did an RFP for both of those systems. Those come back in and then we compared and contrasted those. After we had done all that, the site visit, and the RFP, we came to a consensus as a team with all the stakeholders and we selected Greenway.
Tell me a bit about the implementation process for both the practice management and EHR.
Since we had so many clinics already up on the legacy system, we felt like the best way to do it was more of a big bang approach. When we brought on the legacy systems I was able to stage it because they were all on paper, so I did one clinic every six weeks. I brought them up on the PM first and then I did the same process and brought up each clinic on the EMR.
But, because they were already all on an electronic medical record, we felt like we needed to do it big bang, so we did all the PM first for two weeks. We created all the schedules, migrated all the patients, and did double entry for about two weeks, scheduling patients in both systems. Then we went cold turkey and everything was in Greenway. Then two weeks after that was done, we did the EMR.
Again, we had migrated as much data as we could. There was very little structured data that could fill in to the same fields, so we did have to re-enter a lot of data. But that happened over time. We obviously weren’t able to do that initially. We migrated all the chart notes and then as the patients came in, we started putting in the new structured data in the new fields in Greenway. Because we had so many sites and doing the big bang, we did bring in contract work from Greenway so that we were able to have support at every site, when we went live.
So you electronically migrated of some of the EMR data?
Yes, as much of it as we could. We were able to get in the progress notes, allergies, and medications. Those were things that we felt like we absolutely had to have, as well as the registration data for the PM side. They weren’t able to migrate any of the scheduling, so we had to rebuild all the schedules.
What about scanned documents on the medical records side?
Well, we never scanned in all the paper record on the legacy system because at that time, we did not have the storage for that. So, we still have paper charts, but since we were on the legacy system for five years all those progress notes converted electronically. Now that we’ve been on Greenway for three and a half years, there’s very little that needs to be done in the paper chart, at least for the existing clinics that we brought up at the time. We do have more scanning to do with the brand new clinics that we have since purchased and with clinics that we had but didn’t bring up at the time. With those they have more scanning to do because they were on paper initially and went from paper to Greenway.
Tell me how you get physician buy-in in terms of you changing the workflow from the old system to the new system and just using the computer in general?
Well initially, they were all on the legacy system before we went to Greenway. But to get a buy-in on the legacy system, it was a lot of one-on-one attention and training with them, and support to help them through all that. On Greenway it’s the same thing: we give them a lot of individual training. We do additional training as Meaningful Use changes have come out. We’ve needed them to step up and do a few more things that maybe they didn’t use to, like check a box, or we will help them with workflow changes so that we can get the reimbursement that we need.
I understand that several of your practices are participating in the CMS comprehensive primary care initiative project for Colorado. Tell me about the decision to participate in the program and what that entails.
The decision was made by our COO. She wanted to see if our family medicine and internal medicine practices could participate in that program. She felt like it would help us in our move towards a patient-centered medical home, which is another direction that we are going. We do have some narrow level contracts that are also geared toward patient-centered medical home and we are moving all of our family practice and internal medicine clinics to patient-centered medical home.
When we did the application to be part of the CPCI initiative, we had to apply for each clinic individually. They did select five of our eleven. We do have some different things that we need to do for those CPCI clinics that’s a little above and beyond what we do for the regular patient-centered medical home clinics. But we are trying to keep things standard across the board. The differences that we do are more for initiatives that are being looked at and tracked on the CPCI level that we are not necessarily tracking on the rest of the patient-centered medical home clinics.
What kind of results are you seeing in terms of the quality of the care that’s being provided, both for the clinics that are part of the CPCI and the regular medical homes?
We feel like we’ve really been able to step up the quality of care that we’ve been able to provide. The CPCI has given us some initial start-up money that we wouldn’t have had if we had stayed with trying to implement patients that are in a medical home on our own. We have used that start-up money to create care coordinator positions that we never had before. They aid the physician by working with high- risk patients and getting the high-risk patients more outside care and better coordinated care that we just didn’t have time to do in the past. Things like follow-up for mental health or abuse, as well as additional follow-up for our patients that have been hospitalized. We just didn’t have the bandwidth beforehand to be able to follow up with all of those patients.
Now we can contact those patients that have been hospitalized and find out how they’re doing. If they need to see the physician we get them in to see that provider in a more timely basis. We have done a better job at trying to make sure we have same day appointments to get our patients in. That’s especially been helpful in our internal medicine clinics because often there had been quite a wait to get in to see some of our providers.
And, we are implementing another analytics system that’s due to come online very soon. All the data’s in and we’re just working on the finishing touches which will allow us to really work with registries and more of our high-risk patients preemptively and be able to call on those patients again. Before we didn’t have the bandwidth to do these things or have some of the analytics capability to find those patients. Now we’ll be able to find them much more easily and then work with them preemptively, before their visit, to make sure that they’ve had the labs that they need, that we’re calling them, that they’re doing their blood pressure checks or their sugars checks for diabetes, or those types of things.
What is the analytics program and does it interface with Greenway?
It’s Wellcentive and it does interface with Greenway. All that data has been loaded in from Greenway. I call it kind of an EMR light, but we will not be documenting with Wellcentive. We are using it for the analytic and the registry portion.
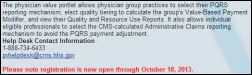
What are some of the things that have made participating in quality initiatives easier because you have an EMR and practice management system in place?
The ability to create structured data and then capture that so that we can track trending issues, follow conditions better, create payment models with the payers, and know beforehand when we’re negotiating those contracts, and knowing that we can meet their requests for the different payment models that are coming.
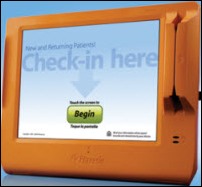
Are you currently using a patient portal?
We’re going to roll it out and start in two weeks. It is from another third party that interfaces through Greenway called Intuit. It is actually live now; we just have not rolled it out to the patients yet. We’re finishing up the legal and the risk assessment on it before we do that.
What is your plan for getting patients to actually use it?
We’re first going to pilot it at two sites, and work with just some specific providers and their care teams. We will, one on one, really try to engage the patient when they’re in there for their visit and see what kind of patient engagement we can have. We’ll let them know that they are part of a pilot so that we can get feedback from them on how we could do it better and determine things that we could improve upon before we roll it out again. Because we have so many clinics, we want to make sure that we do a good job and really make it useful for our patients.
Well, I just want to throw in here, quell some of our provider fears around the portal as well. Our providers are very anxious that it will increase their workload, as opposed to just changing their workload and the way that they’re seeing some things.
Tell me about the innovation award you recently won from Greenway. What specifically was the practice being recognized for?
I think for the way that we are using Wellcentive to meet the needs around patients at our medical home and CPCI. And, from a Greenway standpoint, we’ve also done some work to help them create a GL utility that they never had before, because being part of a hospital system, we have a much more in-depth need for GL than they had ever run into before. As well as our recent implementation of our occupational health clinic and Boulder Center for Sports Medicine using Greenway. Again, therapies that they had not used in the past on their system. And we’ve done it quite successfully; they’re doing really well.
Anything else that you’d like to add or advice that you’d like to give other practices looking to increase their use of technology?
Some of our lessons learned were related to working with a vendor that had not been used to something quite our size. We did have some early growing pains with the way we were scoped from a server size. We didn’t have an adequate number of servers and so we experienced some system slowness that could have been prevented had that been done better. As well as load balancing – just more some technical things that maybe we didn’t scope or communicate as effectively with the vendor as we needed to.
Another lesson learned that we picked up is because we did the big bang and we brought in all the outside contractors that they didn’t necessarily buy into our processes and our workflows. So, there was some subterfuge there when they would be in the clinic and we’d ask them to do things ABC; as they’re rolling them out, the staff would ask questions and they’d go, oh, well, you can just do it CBA. You can reverse the order and it’ll work fine in Greenway. Which is true, but that’s not our workflow, to make sure that things aren’t forgotten and that we’re following all the processes that we need to mitigate patient risk or things like that. So that’s again another lesson learned: to have those people for support on the same page.








The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…