News 8/20/13
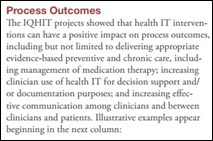
The AHRQ examines the findings from more than 20 studies that were funded by the agency’s Ambulatory Safety and Quality program and concludes that the use of HIT in ambulatory care settings has a positive impact on evidence-based preventive and chronic care delivery, chronic disease control, provider satisfaction, and health outcomes.
Southern New England Ear, Nose, Throat and Facial Plastic Surgery Group (CT) selects ChartLogic’s EHR suite for its 11 physician practice.
More companies are purchasing cyber insurance to cover potential losses and fines in the event of a cyber security breach. About 32 percent of healthcare organizations now have some sort of cyber insurance policy in place and an additional 41 percent are considering purchasing coverage. Industry experts note that in the last six to nine months more smaller practices are expressing an interest in coverage, especially as more data breaches are being publicized and fines are accessed.
The 11-provider Orthopaedic Associates of Augusta (GA) selects SRS EHR.
Physicians across all organizations can expect an average salary increase of 2.4 percent in 2014, which is on par with last year. Physicians in group practices can expect the largest pay increases at 3.7 percent; hospital-based physicians will see increases of only about 2.2 percent.
The most useful patient record strikes a good balance between structured data and a physician’s narrative according Lesley Kadlec, director of AHIMA’s HIM Practice Excellence. Kadlec notes that EHR templates are a great tool but don’t always support good documentation, so she recommends the smarter use of free text and/or the use of speech recognition technology.
Email Inga.
















The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…