News 6/18/13
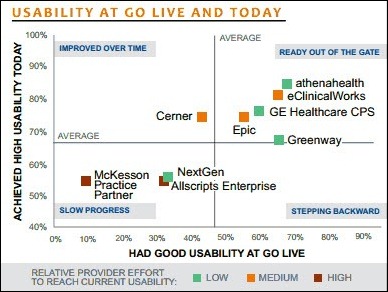
From RyanS: “Re: KLAS Mid-Term Report. Physician’s Computer Company earned the top customer satisfaction scores in both the ambulatory PM and EHR software categories.” The Mid-Term report is based on performance scores gathered over the previous 12 months. RyanS provided a few other highlights, including:
- PCC Partner PM (1-10 physicians) blew away the practice management competition with a score of 95; Epic Resolute/Prelude/Cadence (> 75 physicians) was next with a score of 88.7; Greenway PrimeSuite Practice (11-75 physicians) was third at 88.6.
- Top performers in the ambulatory EMR segment were PCC EHR (1-10 physicians) with a score of 95.5; EpicCare Ambulatory (over 75 physicians) at 88.3; and SRSsoft EHR (11-75 physicians) at 86.7.
- Top clearinghouse providers were Navicure (92.3), ZirMed (92.5), Office Alley (91.1), and Practice Insight (90.1).
- KLAS recognized McKesson Practice Partner (11-75 physicians) as the product demonstrating the biggest improvement since its December, 2012 awards, jumping 13 percent to 56.7. AdvancedMD EHR (1-10 physicians) gained 12 percent to 76.2.
Vitera Healthcare Solutions announces that it has acquired Birmingham, AL-based SuccessEHS, which offers PM/EHR, electronic dental record, dental imaging, and revenue cycle solutions. SuccessEHS, which has doubled in size in the past two years, will be operated as a division of Vitera and expand Vitera’s user base to 10,500 organizations, 415,000 medical professionals, and 85,000 physicians.
CureMD offers discounted subscription rates, and free implementation, training, and data migration for the 4,400 users of the Mitochon Systems EHR platform. Last month Mitochon announced it was exiting the physician EHR market and would no longer market its free EHR product.
The office manager for Summersville Pediatrics (SC) shares her practice’s experience migrating from MyWay to Aprima Medical’s EMR with assistance from Aprima dealer ConXit Technology Group.
CareCloud hires Tom Cady (athenahealth) as VP of professional services.
Nature Coast ACO (FL) expands its relationship with eClinicalWorks to include eCW’s Care Coordination Medical Record.
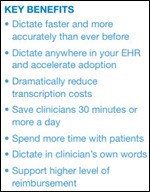
Nuance releases a new version of Dragon Medical Practice designed for smaller practices that includes voice shortcuts to aid searches for medical information and more than 90 specialized medical vocabularies.
A computer outage in the Canadian province of Alberta caused about 202 medical clinics to lose access to patients’ health information for more than five hours last week. “Thousands” of patients were affected and many practices turned patients away. One physician told a local paper, “When this happens it cripples you. We didn’t even have Internet access. This is also a financial loss for physicians.” The EHR vendor blames the outage on a faulty network device that routes data to the clinics.
e-MDs relocates and expands its headquarters and will operate out of a 30,000 square foot administrative campus in Cedar Park, TX, a 40,600 square foot technology campus in Austin, TX, and a separate data center providing business continuity and disaster recovery services.
Vitera Healthcare releases Vitera Medical Manager EHR, a Web-based EHR, analytics, and transaction platform for current Vitera Medical Manager customs.
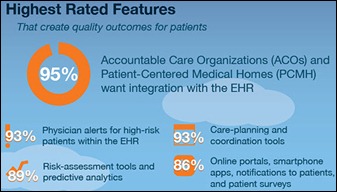
The primary motivator for becoming an ACO or PCMH is to improve patient outcomes, according to a survey by eClinicalWorks. Almost all respondents believe that an integrated EHR would be the most valuable HIT feature for an ACO or PCMH.
An MGMA report provides more evidence that ICD-10 readiness is moving slowly. The greatest concern is the lack of communication and critical coordination between physician practices and their EHR/PM/clearinghouse vendors regarding software updates and testing. Less than five percent of practices report they have made significant progress when rating their overall readiness for ICD-10 implementation.
Emdeon acquires Goold Health Systems, a provider of pharmacy benefits and related services to state Medicaid agencies.
Forty-two percent of practicing physicians are dissatisfied with their jobs, leading many to consider leaving medicine and taking early retirement. Decreasing autonomy, low reimbursement, and administrative hassles were the key drivers of dissatisfaction.
The number of retail medical clinics is predicted to climb from 1,418 at the end of 2012 to 2,868 in 2015.
In an AAFP News interview, Farzad Mostashari, MD discusses EHRs, ROIs, productivity, improved patient care, and more. Regarding productivity:
If physicians just replicate the existing paper-based processes in a digital way, they probably are not going to get huge productivity gains. But if they redesign the care flow to designate what things are done by people versus what’s done through the EHR technology, then that really adds to productivity. That’s how I would summarize the experience of folks who have made EHR implementation a wonderful business decision.


















The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…