News 5/9/13
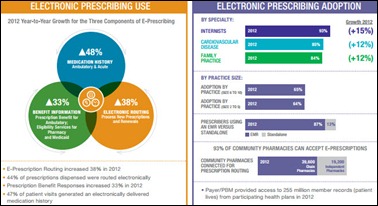
Surescripts releases its 2012 National Progress Report on e-Prescribing, which showed a 38 percent jump in e-prescribing routing from 2011. Other highlights:
- 489,000 (69 percent) of office-based physicians actively prescribed in 2012, compared to 390,000 in 2011.
- Nearly half of patient visits generated an electronically delivered medication history, up from 31 percent.
- 98 percent of chain pharmacies and 85 percent of independent pharmacies accepted e-prescriptions.
- Internists led other specialties in e-prescribing rates at 93 percent, followed by cardiologists (85 percent), family practice physicians (84 percent), and endocrinologists (84 percent).
The 75-physician Tennessee Oncology selects Navigating Cancer’s Patient Engagement Portal.
Allscripts will add 350 new jobs over the next five years in Raleigh, NC as it consolidates its US engineering centers. State officials will extend up to $5.35 million in incentives if Allscripts meets investment and hiring goals, plus maintains the 1,266 jobs currently in Raleigh. The company is expected to invest $2.8 million to expand its Raleigh facilities.
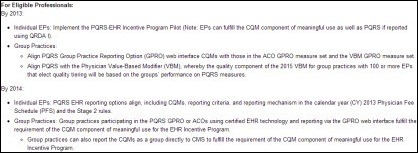
CMS creates a timeline for aligning quality measurement and reporting for multiple initiatives. CMS notes that for 2013, individual EPs can implement the PQRS-EHR Incentive Program Pilot. By 2014, CMS says the PQRS EHR reporting options will align, including CQMs, reporting criteria, and the reporting mechanism in the 2013 physician fee schedule and Stage 2 of the MU program. CMS has provided additional timelines for eligible hospitals and for group practices.
J.M. Winston Radiology Associations (PA) contracts with McKesson Revenue Management Solutions for billing and compliance services.
PerfectServe launches DocLink, a HIPAA-compliant network for texting, voice messaging, and physician-to-physician communication.
Amarillo Legacy Medical ACO (TX) selects eClinicalWorks Care Coordination Medical Record to advance its ACO objectives and coordinate care among its 100+ provider members.
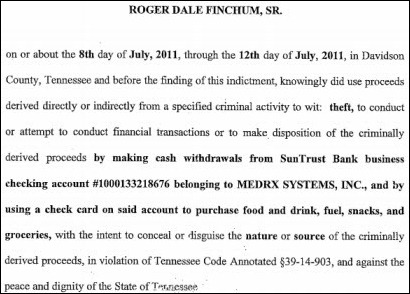
A former director for Tennessee-based EHR developer MedRx Systems is indicted for stealing more than $60,000 from the company in 2011. Roger Finchum, Sr. is accused of making a cash withdrawal from the company’s checking account and using a company check card to purchase food, drink, fuel, snacks, and groceries. A quick Google search reveals that Finchum has been accused of participating in various scams in recent years.


















The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…