News 10/2/12
From Adam Wright: “Re: e-MDs. They laid off 10 of their staff in operations and a couple of sales folks. Something is going on there.” Unverified. We asked e-MDs to comment but did not hear back. [Statement from e-MDs as of 10/3/12 ] “As of October 1st of this year, e-MDs is pleased to report its continuing consistent pattern of year-over-year overall revenue growth. Compared to last year, e-MDs has a greater number of customers and employees, a larger number of contractors, as well as increased revenue. As a general rule, e-MDs does not comment on individual personnel changes that occur during routine business operations.”
My company was “Acquired” today.. 15 years being the middle size guy who bought up small guys. Now we got gobbled bizjournals.com/pittsburgh/new…
— Susanne Bowyer (@2weety13) October 1, 2012
McKesson signs a definitive agreement to acquire MED3OOO. The companies say that once complete, the acquisition will complement the medical billing and PM offerings of McKesson Revenue Management Solutions and accelerate expansion into growth markets, including domain expertise, services, and technologies for building ACOs. I suspect McKesson also found InteGreat EHR superior to its warehouse of legacy EHR offerings, both in terms of technology and scalability for large practices.
PDX-NHIN, a pharmacy management solutions and services provider, will deliver medication histories from its electronic pharmacy record to Emdeon Clinical Exchange, giving providers real-time access to data for medication reconciliation.
Michigan Orthopaedic Institute selects SRS EHR for its 17-provider practice.
Florida International University incorporates the use of CareCloud Charts EHR into its masters program in Health Informatics and Management Systems. Speaking of CareCloud, the company wins an award for Product/Service of the Year in the South Florida Business Journal’s Entrepreneur Awards 2012.
The 90-physician Collom and Carney Clinic Association (TX/AR) chooses MModal Fluency Direct, a speech recognition solution for clinical documentation.
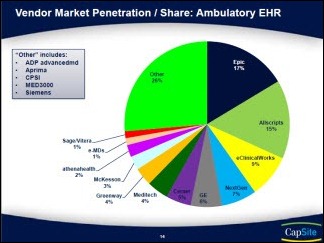
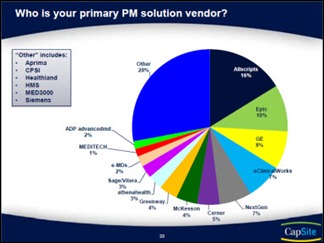
Capsite releases its 2012 Ambulatory EHR and PM Study. Some highlights:
- Epic holds 17 percent of the ambulatory EHR market, followed by Allscripts (15 percent), eClinicalWorks (nine percent), and NextGen (seven percent)
- Allscripts is the leading PM vendor with a 16 percent market share, followed by Epic (10 percent), GE (8 percent), and eClinicalWorks (seven percent)
- 40 percent of organizations are in the market for an EHR and most will buy within two years
- Only 27 percent of organizations intend to buy or upgrade their PM system
- 43 percent say they have successfully attested for Stage 1 MU; an additional 23 percent aren’t sure of their MU attestation status
- Almost half of organizations plan to join an HIE.
AAFP News Now explores an emerging struggle for practice owners and employed providers: how to allocate MU funds, shared savings, and new quality-based incentive payments. Unless addressed in an employment agreement, employed providers are entitled to their own MU incentives, even if they did not pay for the EHR. The advice: new employment agreements must address bonus opportunities, performance expectations, and the distribution of financial incentives.

















The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…