HIStalk Practice Interviews John McConnell
John McConnell is president and owner of McConnell Golf. He co-founded Medic Computer Systems (acquired by Misys in 1997 for $923 million, now part of Allscripts) and was chairman and CEO of A4 Health Systems (acquired by Allscripts in 2006 for $272 million).

You left Allscripts and the HIT world four years ago. What have you been doing since then?
I started McConnell Golf in 2003 when I purchased Raleigh Country Club while also being CEO of A4 Health Systems. After that company’s sale to Allscripts in 2006, I wanted to pursue a new industry challenge and have focused on growing McConnell Golf. Today we own eight clubs and employ over 500 people. McConnell Golf hosts the Wyndham Championship, which is a PGA event at one of our clubs in August, as well as a Nationwide Tour event in June.
Do you think today’s business and HIT environment could support startup companies similar to the ones you built with Medic and A4?
There will always be room for new companies and new products. At Medic, we developed most of our products when I was with that company. At A4, we were much smaller than Medic and other competitors, so we acquired other businesses with established technology in order to get to market faster at lower costs.
I see the same opportunities today for smaller businesses to be acquired by larger HIT entities due to time and the research and development investment required to create and execute on new ideas. On numerous occasions, I am asked to review new products that small startups are developing, and many are very good ideas that can fulfill a niche in HIT. Certainly I think developing large-scale, enterprise-wide solutions would not be the best place for small companies to invest and compete today.
If you were starting an HIT company today, what area would you choose?
Analytics. Information from the various HIT systems tied together to help reduce costs, eliminate service redundancy, identify fraud, and improve patient care will be huge.
Is healthcare software becoming as commoditized as hardware?
Most mature systems are very comparable today, and I see a continued lower-margin business for most of the vendors in their software sales. Service revenue is the future for most HIT companies, which is similar to how IBM moved from hardware into consulting as margins in their historic business eroded.
The same business rules apply today as in the past. Those companies that can gain customers with efficient marketing and implement their solutions in a timely and cost-effective manner will gain market share. Pricing will continue to drive a lot of buying decisions. Web-based solutions are quicker to build, implement, and maintain, so lower pricing should be the norm for the customers.
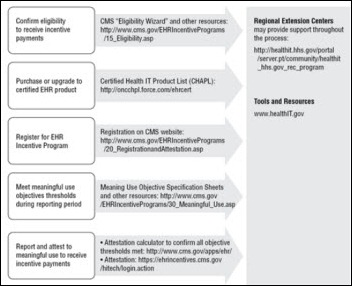
What are the good and bad aspects of Meaningful Use?
I think Meaningful Use will help control the ongoing rise in healthcare costs going forward if it is given time to succeed. Having greater automation and less paper will be good for everyone. Technology helps reduce costs and errors in delivering healthcare services, so those are positive benefits.
Bad aspects may be that caregivers spend more time documenting and looking at computer screens than with the patients. I also see the trend for the older physicians to retire sooner than later as their reimbursements are reduced further by not implementing technology.
Who in the industry do you really admire?
My top three in no order of preference are Neal Patterson from Cerner, as he had a long-term vision for HIT and never let the Wall Street crowd interfere with it. I admire Judy Faulkner at Epic because of her emphasis on software, company culture, and maintaining the private company status. Patrick Hampson at MED3OOO has reinvented that business at least three times from its founding in 1995 to adapt to industry dynamics, so that takes sincere leadership skills.
What ugly lessons did you learn running publicly traded companies?
The biggest issue that I found for myself personally was that I started managing the business to meet Wall Street expectations instead of our customer ones. Each quarter end became challenging for our business and employees because of the pressure and pride we felt not wanting to lose any money for investors that bought our stock. Quite honestly, that caused us to make some poor business decisions in granting discounts or other incentives to our prospective customers at quarter end that we most likely would not have offered as a private business.
Today I sit on one public board, and the government regulations now in place for public companies are very challenging and expensive to manage. Personally, I also see more investors looking for short-term results in stocks that they buy instead of valuing the company’s long-term potential. However, even with the negative issues that I have outlined, public markets provide valuable capital to businesses to grow to new levels that benefit many.
Allscripts is in the midst of a rough patch with its recent board turnover, missed earnings, and drop in stock price. Do you think this is just a bump in the road or do you predict more turmoil in coming months?
I have been off the Allscripts board since 2008, so my familiarity with the business is not very current. Their management team has certainly built an impressive business in both revenues and customers, so they enjoy a very strong position in the industry.
Integrating large acquisitions and different product lines in a short period of time will be challenging for any company. That is most likely the major reason why Allscripts recently hit a bump in the road in their business financial results and significant loss of shareholder value. With any board, you often have diverse opinions on the business strategy to pursue, so that can create major conflicts among its members.














The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…