News 3/29/12
NextGen enters into a reseller agreement with Nuance, giving NextGen the opportunity to sell Dragon Medical speech recognition software directly to its Ambulatory EHR clients.
Speaking of NextGen, I see they are hosting their fifth annual NextGen Cares Golf Tournament April 23rd in Horsham, PA benefiting the Jayne Foundation.
Online physician networking site Sermo names former Revolution Health president Tim Davenport CEO. Davenport replaces Sermo founder Daniel Palestrant, who left the company in January to run Par80, a start-up focused on improving the patient referral process.
The Centricity Healthcare User Group hosts its annual meeting April 20-21st in Las Vegas. CHUG is not an official organization of GE Healthcare and the group limits its membership “to well-behaved licensed Centricity EMR users, GE Healthcare employees, and a few very polite consultants and vendors of products supporting Logician.” I wonder if CHUG expects everyone to remain “well-behaved” and “very polite” while visiting Sin City.
Greenway Medical makes its PrimeMobile clinical and financial application available for Android smartphones and table devices.
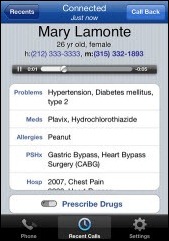
Cool-sounding technology: Giffen Solutions launches MexCom, a smartphone app that will record, transcribe, and archive conversations. The app also allows physicians to access a patient’s health profile when a patient calls and to e-prescribe. I didn’t see anything on their Website to suggest it interfaces with a practice’s EMR but otherwise the functionality looks handy.
The American College of Osteopathic Family Physicians names MDdatacor its vendor of choice to offer the College’s Medical Home Quality Markers program. The program will use MDdatacor’s technology platform for patient data management and reporting for members seeking PCMH recognition from NCQA.
A physician with Northwestern Memorial Physicians (IL) resigns earlier this month, blaming the practice for “technology troubles, billing errors, and lack of adequate office staffing.” Northwestern, which utilizes Cerner, rejected the resignation, claiming that Dr. David Vigder breached his employment contract and improperly engaged in talks with the practice’s chief competitor, NorthShore University HealthSystems’s Medical Group. Vigder responded through his attorney, providing details of the “severe computer problems” that made communication with specialists difficult. Northwestern has subsequently responded to Vigder with a lawsuit. Stay tuned.
In an interview on Fox Business, athenahealth CEO Jonathan Bush discusses the need to get doctors to believe in the Cloud; he also shares impressions on the healthcare reform debate.
TransforMED, the AAFP subsidiary dedicated to helping organizations adopt the PCMH model of care, expands its leadership team and staff. In addition to the hiring of several project managements and practice enhancement facilitators, TransfoMED names Barbara Doty, MD and Laura Knobel, MD to its board of managers and promotes Diane Cardwell to VP of healthcare solutions and Dan McKean to VP of business development.
Two practices within the University at Buffalo School of Medicine select PatientKeeper Charge Capture, which will be integrated with UBMD’s GE Centricity Group Management PM product.
CalOptima REC reaches it 1,000 member enrollment goal for primary care providers.




























The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…