News 12/7/10
Healthcare communication provider NaviNet acquires Prematics, a developer of mobile clinical messaging and e-prescribing tools. NaviNet will integrate the Prematics mobile care management products with NaviNet’s Insurer Connect, EMR, and PM solutions.
Industry consolidation continues. The 23-doctor New Hanover Medical Group (NC) joins New Hanover Regional Medical Center’s owned physician group. The arrangement gives the New Hanover Medical Group access to the hospital group’s business support, including medical office technology, quality resources, and contract negotiations.
eDoctor and X-Med partner to integrate eDoctor’s ePrescribing into X-Med’s Linux-based PM system.
The 50-provider Ear, Nose and Throat Associates of South Florida picks PatientPoint’s RCM and self-service offerings to run with its existing PM and EMR.
The Eye Care Institute (KY, ID), completes its conversion to MedFlow EMR.
Sisters of Charity Health System (OH) launches an IPA, designed to provide a platform to offer additional services to its independent physicians. The IPA will offer GE Centricity’s Practice Solution, billing and collection services, consulting, and managed care contracting.
In a study published in Clinical Transplantation, researchers finds that an electronic monitoring system and personalized counseling help improve medication adherence rates for kidney transplant recipients. Medication adherence jumped 40% when patients were given personalized phone counseling, along with prescription bottles that used integrated microcircuits to record when medicine was taken.
On other hand, an automated call-in system to monitor heart failure patients failed to show benefits, according to a NEJM study. Participation was apparently an issue, with 14% never using the telemonitoring system and only 55% calling in at least three times a week after six months.
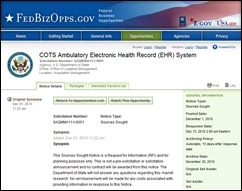
The Department of State is hunting for an ambulatory EHR system to use in its medical offices across the world, including US embassies and consulates in 170 countries. Interested vendors must respond by December 15th.
I was intrigued by this press release, issued by the 800-physician member Brown & Toland (CA). Allscripts CEO Glen Tullman tells 100 Brown & Toland doctors that their organization is well positioned for success as an ACO, based on its early adoption of EHR technology. The release provides additional details of the Allscripts systems that is currently or in the process of being implemented. I’m assuming Brown & Toland is targeting non-member physicians with this message in hopes of recruiting more providers. The San Francisco-based Brown & Toland is headquartered in a highly competitive healthcare market and likely needs plenty of troops, assuming it wants to hold its own in the ACO alignment race.
New technology alert: Mobisante is beta testing a handheld ultasound device that connects to a cellular network or Wi-Fi, allowing users to immediately send images to other providers. The company hopes the market will be drawn to the product, based on its flexible connectivity options and portability. Mobisante is waiting for FDA clearance and hopes to start commercialization in 2011.
Good news for family practice docs. Medicare allowances continue to rise for CPT codes 99213 and 99314, which represent 84% of all FP office visits by established Medicare patients. In 2006, 99213 paid $52.06; in 2011 payment is projected to be $74.85. Similarly a 99214 routine office visit earned $82.62 in 2006 and will pay $111.36 in 2011. Yes, good news, indeed, but still a lean living compared to specialists.













The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…