Note: you can download a handy PDF of this page to take along to New Orleans.
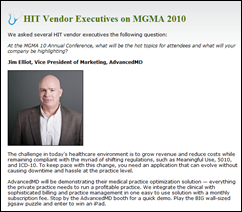
Advanced MD Software
Booth 1628
10876 South River Front Parkway
Suite 400
South Jordan, UT 84095
Phone:801.984.9500
www.advancedmd.com
Announces a new, fully integrated EHR + PM/RCM solution. Physicians gain the benefits of strong EHR with integrated ePrescribing and pre-built, customizable templates. Office managers gain access to a strong claims management system, payer-rules engine, and simple denial tracking. Designed to support the needs of medical practices and billing services.
Allscripts
Booth 1417
222 Merchandise Mart
Suite 2024
Chicago, IL 60654-1034
Phone:919.329.1070
www.allscripts.com
Allscripts (NASDAQ: MDRX) provides innovative solutions that empower all stakeholders across the healthcare continuum to deliver world class outcomes. The company’s clinical, financial, connectivity, and information solutions for hospitals, physicians, and post-acute organizations are the essential technologies that enable a connected healthcare community.
Culbert Healthcare Solutions Inc
Booth 142
800 West Cummings Park
Suite 6000
Woburn, MA 01801
Phone:781.935.1002 ext. 13
www.culberthealth.com
Culbert Healthcare Solutions is a professional services firm serving healthcare organizations. We specialize in helping group practices leverage clinical and practice management technologies to improve patient care and financial performance by implementing best practices.
eClinicalWorks LLC
Booth 1536
112 Turnpike Road
Suite 200
Westborough, MA 01581
Phone:508.836.2700
Fax:508.836.4466
www.eclinicalworks.com
eClinicalWorks provides ambulatory clinical solutions, including EMR/PM software, patient portals, and community health records applications. With 40,000+ providers and 120,000+ medical professionals across all 50 states using its solutions, customers include small, medium, and large physician practices, outpatient departments of hospitals, health centers, departments of health, and convenient care clinics.
e-MDs
Booth 1207
9900 Spectrum Drive
Austin, TX 78717
Phone:8888.344.9836
www.e-mds.com
e-MDs is a leading developer of healthcare software solutions, founded in 1996, and actively participates in national health information technology and interoperability efforts. e-MDs Solution Series is the standard for affordable, integrated EHR/PM solutions, including clinical, financial, and document management modules that automate medical practice processes and chart management.
Greenway Medical Technologies
Booth 517
121 Greenway Boulevard
Carrollton, GA 30117
Phone:770.836.3100
www.greenwaymedical.com
Greenway Medical Technologies, Inc. provides a complete physician’s infrastructure of clinical, financial, and administrative technologies through its integrated, single-database EHR, practice management, and interoperability solution PrimeSuite. Greenway’s certified and KLAS-award winning solutions serve more than 23,000 healthcare practitioners nationwide in 30 specialties and subspecialties.
iMDsoft
Booth 1504
300 First Avenue
Needham, MA 02494
Phone:781.449.5567
www.imd-soft.com
The iMDsoft MetaVision Suite of clinical information systems features fully-integrated tools for data collection, presentation, order management, and decision support across the critical care and preoperative continuum.
Ingenix
Booth 724
12125 Technology Drive
Eden Prairie, MN 55344
Phone:888.345.8745
www.ingenix.com
Ingenix CareTracker is 2011 CCHIT-certified EHR/PM solution that is guaranteed to help physicians meet meaningful use requirements. It’s built with cloud computing technology so you get instant updates, reliable accessibility, complete global content, and immediate connections to labs, pharmacies, and hospitals — all for a lower total cost of ownership.
McKesson
Booth 618
5995 Windward Parkway
Alpharetta, GA 30005
Phone: 404.338.3807
Fax: 404.338.5121
www.mckesson.com
McKesson delivers solutions to physician practices of all sizes and specialties, providing physicians with more products, services, and resources than any other healthcare company — including practice management systems and EHR, billing and accounts receivable management and connectivity services, medical supplies and equipment, and pharmaceuticals.
MED3OOO
Booth 844
680 Andersen Drive
Foster Plaza 10
Pittsburgh, PA 15220
Phone:412.937.8887
Fax:412.937.9221
www.MED3OOO.com
MED3OOO, experts in healthcare management and information technology, advances performance of group medical practices, clinics, and hospital-employed physicians with RCM and ASP PM/EHR systems. Stop by our booth for a demonstration of our InteGreat EHR the intuitive browser-based solution. Uncover your practice potential with MED3OOO’s team of experts.
MedAptus
Booth 702
176 Federal Street
4th Floor
Boston, MA 02110
Phone:617.896.4000
Fax:617.482.1110
www.medaptus.com
With the most powerful, yet easy-to-use, Intelligent Charge Capture technologies available, MedAptus enjoys enterprise-wide adoption at many prestigious, academic healthcare organizations. Our full-scale Professional and Facility offerings increase revenue, re-engineer archaic processes, enhance EMR investments, and save busy providers time.
Medicity
Booth 1644
56 East Broadway #600
Salt Lake City, UT 84111
Phone:801.322.4444
www.medicity.com
Medicity’s care collaboration solutions work the way you do. We connect you to colleagues, service providers, hospitals, and patients on your terms — without disrupting your workflow. Coordinate care around a 360° view of your patients’ health through the largest network of connected providers in the nation. Are you iN?
Navicure Inc.
Booth 1046
2055 Sugarloaf Circle, Suite 600
Duluth, GA 30097
Phone:770.342.0200
www.navicure.com
Navicure is an Internet-based medical claims clearinghouse that helps physician practices increase profitability through claims reimbursement and staff productivity. Our solutions automate account receivables processes, including patient eligibility verification; primary and secondary claims reimbursement; rejected and denied claims management; electronic remittance and posting; claims and remittance reporting and analysis; and patient statement processing.
NextGen Healthcare
Booth 1136
795 Horsham Road
Horsham, PA 19644
Phone:215.795.1050
www.nextgen.com
NextGen Healthcare is a leading provider of integrated electronic health record and practice management systems, connectivity solutions, and billing services designed to serve the needs of ambulatory practices and hospitals of all sizes and specialty areas. Our award-winning, certified solutions help improve care quality and increase operational efficiencies.
Nuance
Booth 535
One Wayside Rd
Burlington, MA 01803
Phone:781.565.5000
www.nuance.com/healthcare
Nuance’s Dragon Medical is the most widely used speech recognition system in medicine today. Dragon Medical reduces transcription expense, delivers results rapidly, and heightens clinician satisfaction by making EHR systems easy to use, which accelerates the adoption of clinical information systems so provider organizations maximize the return from IT investments.
PatientKeeper
Booth 541
275 Washington Street
2nd Floor
Newton, MA 02458
Phone:617.987.0300
www.patientkeeper.com
PatientKeeper works with hospitals and physicians to deliver a single place to work. Through integration and workflow optimization, PatientKeeper has the highest physician adoption rates in the industry. PatientKeeper’s solutions ensure that HITECH meaningful use criteria are met. PatientKeeper’s return on investment is demonstrable and proven across our client base.
RelayHealth
Booth 128
1145 Sanctuary Parkway
Suite 200
Alpharetta, GA 30004
Phone:510.637.7722
www.relayhealth.com
With market-leading clinical, financial, and patient connectivity solutions, RelayHealth provides the access and tools to improve patient care, enhance financial management, and interact with patients and other healthcare providers. Put these advantages to work for you and experience the benefits of Health Connections Brought to Life.
Sage
Booth 536
4301 West Boy Scout Blvd., Suite 800
Tampa, FL 33607
Phone:877.932.6301
www.sagehealth.com
Sage provides physician practice management and electronic health records software and services for small to medium-sized practices as well as enterprise customers. We combine business management tools with technology and information solutions that transform both the clinical and financial aspects of healthcare delivery.
SRSsoft
Booth 1101
95 Chestnut Ridge Road
Montvale, NJ 07645
Phone:201.802.1300
Fax:201.802.1301
www.srssoft.com
For over a decade, SRS has been the leading provider of productivity-enhancing EMR technology. The powerful SRS Hybrid EMR delivers speed, enhanced revenue, and client satisfaction. Valued by high-performance physicians, it is particularly well suited to the needs of specialists. Its successful adoption rate is unparalleled in the industry.
ZirMed Inc.
Booth 838
888 West Market Street
Louisville, KY 40202
Phone:877.494.7633
www.zirmed.com
ZirMed is a nationally recognized leader in delivering revenue cycle management solutions to healthcare providers. Through the integration of its proven healthcare EDI solutions with powerful healthcare analytics and smart financial services, ZirMed enables healthcare providers to leverage the power of technology to cure administrative burdens and improve cash flow.























The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…