Intelligent Healthcare Information Integration 9/25/10
POF, POOF, POTF — It’s All Geek to Me
Just days after last year’s American Academy of Pediatrics National Conference and Exhibition (AAP-NCE) in Washington, DC, we began to work on this year’s “Pediatric Office of the Future” exhibit. Trying to showcase technology capabilities for pediatricians in an educational, yet exhibit hall-style show has become a year-round challenge. (I’d call it a “job” instead of a “challenge” except that would imply at least a modicum of pay.)
It’s really a labor of love — though some have said it’s more of “insanity” — trying to engage medically-oriented ,tech-savvy companies of all sorts and sizes into donating time, people, resources, money, and prizes. It becomes exceptionally tricky when you need them to understand that while we appreciate their desire and need to generate sales leads — they are in business to sell products and/or services, for sure — in our exhibit, we need them to keep the educational focus at the fore. We want our sponsors to find value for their generosity, but our booth is all about the attendees getting an education regarding currently available “future” technologies. (Yeah, I know, but “Pediatric Office of the Nowadays” just doesn’t sound as zippy.)
Speaking of names, I get a whole heap of variations on the acronym, or the assumptions thereof — POF, POOF, POTF, etc. We have always used the shortest, POF, but take your pick. “Call us what you will, as long as you call us!”
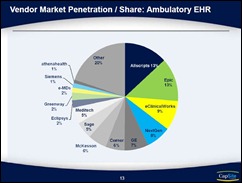
The team has really put together an impressive “show” for 2010. (Be warned: blatant POF promo approaching!) Our 30’ X 30’ booth now has displays and sponsors on every inside and outside wall…and beyond! We have some of the biggest names in EHRs and HIE, some really great tools for practices, “green” tech, non-brick-and-mortar office ideas, cool health literacy tools, and even an international “tech head” from eastern Africa bringing MIT Sloan along for the ride. Plus, we have been successful in organizing a side bar to the POF: the “Future Faces Family Fun & Fitness Zone.” We have grown way beyond our four walls and now have the second largest footprint in the exhibit hall!
The AAP has shown us lots of love, both in onsite as well as pre-show marketing. We have even been given our own Web presence, something rather unusual for such an event, at http://aapexperience.org/future. Details of all our generous sponsors and their educational foci as well as links for more of their details are there. Also, you can read more about the “Future Faces” fun stuff (i.e., games, “Eye Screen for Ice Cream,” enjoyable distractions for kids of all ages, etc.) Not the least important, you can also see a list of the over $40,000 in prizes we have been generously provided which we’ll be giving away over the three days of the exhibit. From an EHR to a hippopotamus to 500 thumb drives and more, attendees who stop by and get their badge scanned are all automatically entered.
Am I trying to sell the POF? You betcha! I love selling it because it doesn’t cost anything for attendees. It’s a “value add.” So, if you’ll be in or around San Francisco October 2-4, come by the Moscone Center and see why I’ve become such an unabashed pitchman. I’m pretty sure you’ll enjoy the “show.”
Oh…one last pitch: we’ve already gotten some huge conversations with some even more gigundo companies interested in sponsorship for the 2011 POF. It’s looking truly legen…wait for it…dary!!!
Back from the future trenches…
“A lie is just a story ruined by the truth.” – Barney Stinson
Dr. Gregg Alexander, a grunt in the trenches pediatrician, directs the “Pediatric Office of the Future” exhibit for the American Academy of Pediatrics and is a member of the Professional Advisory Council for ModernMedicine.com. More of his blather…er, writings…can be found at his blog, practice web site or directly from doc@madisonpediatric.com.













The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…