Intelligent Healthcare Information Integration 4/17/10
AAs for EHRs
No, this isn’t an offering from Bill W, nor is it a Serenity Prayer for EHRs. (Though I could use one of those some days!) This is about the two main players acting upon providers when it comes to EMRs: aversion and attraction. It’s about what can draw doctors toward, and what will repel them from, digital healthcare data use and adoption.
Attraction:
· Ease of use
· Ease of use
· Ease of use
Think “apps.” There’s not one non-geekified physician out there who wants anything to do with learning about dropdown boxes, navigation panes, or data input modalities, no less any who care one whit about programming language limitations or whether it’s MySQL or yours.
Docs want to see patients. It’s that simple.
We never wanted to become data collection devices assisting insurance company profit margins nor defensive documenters dodging ambulance-chasing lawyers looking to capitalize upon the imperfections inherent in being human.
So, give us easier ways to practice medicine. Period. Do that and docs will literally flock, in mass migratory waves, to your door.
Aversion:
· Clicks
· Clocks
· Clacks
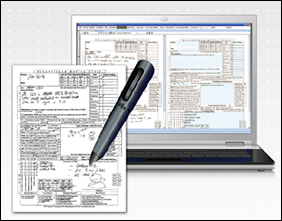
Clicks, also known as “clicky-clicks,” is shorthand for all the monstrously difficult ways we’ve thus far devised for interacting with computers. Compared with pen and paper, few information input methods can be called anything but regressive. (OK, voice recognition has gotten good, but it’s still tough to do in a noisy, busy office.)
Clocks are the continually ticking timepieces running doctors’ professional lives. Lower reimbursement leads to the need to see more patients, but more regulations require more data collection which takes more time per patient. More times more times more equals less: less time available, less fun, less happy providers, mathematically proven here:
A clack is defined as both “thoughtless, prolonged talk” and “a simple valve allowing one-way flow.” Both definitions fit many of the tasks associated with EMR use and adoption. Think about it.
Minimize the clicks, enable slower clocks, cut out the clacks and, again, physician flocking will occur.
This isn’t about the incentive dollars which will be gone before we know it. If vendors and governments want docs to adopt, understand and address the AAs of EHRs and help us get flocked.
From the flocking trenches…
“A word to the wise ain’t necessary – it’s the stupid ones that need the advice.” – Bill Cosby
Dr. Gregg Alexander, a grunt in the trenches pediatrician, directs the “Pediatric Office of the Future” exhibit for the American Academy of Pediatrics and is a member of the Professional Advisory Council for ModernMedicine.com. More of his blather…er, writings…can be found at his blog, practice web site or directly from doc@madisonpediatric.com.






The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…