EMR Vendor Executives on Meaningful Use and Certification Requirements – Part Two of a Series
We asked several vendors a series of six questions related the federal government’s recent announcement on the latest proposed meaningful use definitions and EHR certification criteria.
Which of the criteria do you expect to be the most difficult for physicians to achieve?
Allscripts – Glen Tullman, CEO
We have heard concerns from a number of physicians, most of whom do not currently use Electronic Health Records, that a few key areas are a concern. Our response is typically that we can show them practices that are very similar to their own who are actually performing the activities in question.
The key areas of concern revolve around the requirement that they enter 80% of their orders in an EHR, since that level of automation requires a significant change in their normal workflow. However, we’re optimistic that physicians using Allscripts EHRs will be successful meeting the measures for order entry. According to a recent KLAS survey, Allscripts was the only vendor with 100% of clients surveyed able to transmit qualifying digital orders. One example is Sharp HealthCare in San Diego, the Malcolm Baldrige National Quality Award-winning health system led by CIO Bill Spooner. Sharp is now placing 100% of their orders electronically using Enterprise, after going live last month in a big-bang implementation of Orders with 350 physicians and 2,000 total users submitting lab and radiology orders using the EHR. So Sharp stands out as a great example of what a world-class healthcare organization with strong leadership and a commitment to success can do to make Meaningful Use work.
Additionally, we have heard physicians are concerned about medication reconciliation – another requirement of the Meaningful Use criteria, as they’re now written. And the requirement that physicians provide “syndromic surveillance reports” is challenging because it remains undefined, untested and unclear. Fortunately, the requirements in this area are fairly minimal, so as long as we facilitate an easy path for testing this for clients, they’ll be successful.
eClinical Works – Girish Kumar Navani, CEO and co-founder
Change is always hard. However, we seem to have a lower and shorter learning curve for our products and services. It is important that we standardize the measures by specialty in a timely manner and the HIT standards group develops a more standardized LOINC mapping for labs.
Eclipsys – Philip M. Pead, President and CEO
The functionality based criteria should be relatively straightforward and are likely part of almost any certified EHR implementation. It’s the Quality Reporting requirements, which require appropriate structured data capture in the EMR and integrated reporting solutions. Additionally, many of the quality reporting standards are undefined, or ill defined that will clearly be a challenge for suppliers and providers – especially as quality indicators become more directly tied to reimbursement, or when the ARRA “carrot” becomes a “stick.”
As it stands, as a whole, the healthcare industry does not currently communicate health information well, nor does it aggregate it well enough to see patterns and find trends. Labor intensive manual reporting is a huge cost for hospitals and it only offers views of past events. It will become increasingly obvious that HIT design needs to not only provide access to data, but also the seamless extraction of data for comparative and quality purposes in order to help providers prove they are meeting the meaningful use requirements.
e-MDs – Michael Stearns, President and CEO
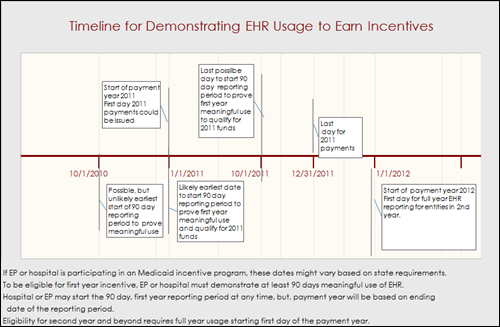
While we feel that none of the proposed criteria are onerous or beyond what current EHR users should already be achieving, the need to implement 5 clinical decision support rules and tracking their compliance might be a challenge to some physicians. The tools in the EHR need to be able to facilitate this process without a substantial increase in administrative overhead. For this reason we were pleased to see that the initial reporting period for physicians was a continuous 90-day period; this gives our clients — particularly physicians who purchase from this point forward — time to implement and stabilize their usage with core functions before optimizing for meaningful use.
GE Healthcare – Vishal Wanchoo, President and CEO, GE Healthcare IT
Certainly a 75% threshold for e-prescribing applicable prescriptions or 80% for CPOE for orders may be challenging for some, especially in that first year of meaningful use, in addition to the requirement for the authorizing provider to enter the order.
For many practices, the biggest challenge, especially given the many high performance goals, will be achieving broad EHR integration into the practice.
InteGreat, a MED3OOO Company – Tom Skelton, President
I believe that having physicians reach the 80% level on order entry will be difficult to achieve. Many physicians have traditionally relied on support staff for this function and having that function shifted to the physician will be a challenge. It is a big behavioral change, and one that requires further direct investment of physicians time in the process.
McKesson – Dave Henriksen, SVP and GM, Physician Practice Solutions
Our physician customers — especially those in rural areas — tell us that they feel that the bar has been set very high for a number of Stage 1 measures, such as: CPOE for 80% of all orders; clinical summaries provided for 80% of all patient visits; and e-prescribing used for at least 75% of prescriptions. These metrics could be particularly difficult for providers in small practices to achieve, as well as for those that are in the early stages of EHR system adoption. We will include this feedback in McKesson’s public comments and hope to see these requirements relaxed so they don’t discourage eligible providers from moving forward with EHR adoption.
NextGen Healthcare – Scott Decker, President
Criteria related to interoperability will likely present some challenges for physicians. Providers have not been given much opportunity to share data across technology platforms in the past, due in part to a lack of market development and in part to technology gaps. We are pleased to be able to highlight several of our clients as examples of where interoperability is functioning effectively and benefiting patients as a result. We feel so strongly about the importance of sharing data across platforms that we designed our data portal — called our Community Health Solution — to be interoperable from its first installation in Ann Arbor, Michigan back in 2005.
Another challenge for physicians in day-to-day practice will likely be in the area of clinical decision support (CDS). There is broad agreement that such tools are key to realizing the promise of safer, more efficient, and higher quality care for all patients. The challenge is in creating and implementing clinical decision support tools that actually support care rather than distract from it. A successful CDS solution must be flexible (as clinical guidelines change and new ones are added, the support tools must be able to to change in near real time), scalable (technical solutions that could work for a small number of static conditions may not be adaptable across all specialties and conditions), and fit into the mental and physical workflow of the user. NextGen Healthcare has worked closely with our clients to create solutions that we believe meet these real world needs for the busy practicing clinician.
A final point of concern will mostly likely be the physician’s ability to share clinical information with their patients, and in return, allow patients to provide information on their health needs back to the physician. Our experience is that most physicians today do not have systems in place that share information with other physicians and/or patients. For the past several years, NextGen Healthcare has been offering a tool to our clients called NextMD, which allows secure online sharing of information between physician and patient. While not intended to be a personal health record, the module does allow confidential sharing of data along the lines of the 2011 requirements.
Sage – Lindy Benton, Chief Operating Officer
Overall, we think CMS and ONC got this one right by setting the bar at “meaningful” but making it incremental and leaving some fluidity in the first year. We don’t really see any of the criteria as being terribly difficult to achieve, at least individually, but anytime physicians are asked to make changes to workflow there’s a potential for some push back. In total, the stage one requirements certainly represent a change in workflow for some providers, depending on their experience with technology and their starting point, but if the goal is improving healthcare at the practice and national level, change is required.
Through our programs and outreach with customers, and throughout our discussions with physicians during the sales cycle, we keep the focus on the goals that physicians have for implementing EHR in the first place, aside from the stimulus. The physician goals — the ones that are “meaningful” to their practices, are often the most attainable. Sage has been implementing EMR/EHR systems for over a decade and e-prescribing for even longer, so we have a lot of experiences to draw from where practices have made changes, achieved real results, and are doing things that closely mirror the proposed definition of meaningful use.
Sage has carefully reviewed the NPRM and IFR and, in addition to drafting our comments, we are analyzing the implications for our company and our customers. At this point, while not overly concerned about anything in the Stage 1 criteria, we are mindful of those requirements that relate to things outside the control of Sage and the physicians using our product. Depending on how it is interpreted and assessed, the requirement to exchange information with other stakeholders could prove difficult in the context of fragmented, proprietary networks. At the same time, meaningful data exchange is key clinical and operational improvements and one of the most frequently expressed goals of our physician customers.
SRSsoft – Evan Steele, CEO
Before answering this question, it is important to note an overarching issue: “meaningful use” means that providers must not only adopt and deploy an EHR, but they must also use it in what the government considers a “meaningful way.” The process of defining use in a “meaningful way” has taken the good part of a year, but essentially it comes down to just one fact — the government wants to tell physicians what data it wants, how it wants it, and when it wants it. It must be provided electronically and at a level of detail that is only partially spelled out at this time. In order for any such data to be provided to the government, virtually all data from every exam, medication, order, prescription, report, and test, along with diagnostic and demographic data, has to be entered into “the system” for each patient and each exam.
This is a huge undertaking and a huge burden for physicians and their office staff. It forces them to enter every single piece of data about the patient, the exam, the outcome, and the follow-up into a computer terminal and screen. Physicians will be forced not just to enter all their exam data, but to become experts in system “navigation” and tedious data entry. This will slow things down considerably– not just initially, but for a long time. It will cause providers to see fewer patients and will have a negative impact on their incomes, especially specialists and high-performance physicians.
The answer to your question is based on the more than 5,000 providers we have as clients, mostly specialists. They will not be able to gather and input this volume of data into the EHR without a negative impact on the number of patients they can see and on their revenue streams. If they choose to participate in ARRA, they will realize a major hit to their bottom lines right away.
Aside from that meta issue, there are still some daunting challenges in the requirements themselves. Two measures are particularly troublesome:
- The requirement to perform even one test of the ability to exchange clinical data between different entities using distinct EHRs is unrealistic, given the current lack of interoperability even between EHRs of the same vendor.
- CPOE is a deal-breaker for most physicians. It is simply too time consuming. Prescription ordering is workable, but only with the right ePrescribing technology. Inputting all of the other orders will not be embraced by physicians.
















The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…