Glen Tullman is CEO of Allscripts.

What kind of companies are winning and losing as everybody waits for HITECH to settle itself out?
I think that HITECH has generally been directed and the bulk of the funding has been directed at the ambulatory area, focused on electronic health records. So what we see as the winners, there’s two factors going on.
One has been the economy, generally, and that has put a crimp on anyone who’s out there doing bond issues, raising money, or the like. Then the second one, in a positive vein, has been the stimulus, which is known as ARRA. That injection — of what was $38 billion, now revised up to $48 billion — has been a positive.
The winners in the space are the ambulatory companies like Allscripts, who are seeing strong interest in electronic health records because physicians know that they can get $44,000 each.
The “losers” — and I want to put quotes around that because I’m not sure there’s going to be any losers in healthcare information technology — but let’s say the folks who are seeing a little slowing of their sales have been the traditional hospital companies. Primarily because the big hospital projects that require bond issues and the like have generally been put on hold and people are more focused on electronic health records.
Then you have a third group of folks who are not typically involved, who are trying to get involved in electronic health records. There are some groups that are trying to say, “Hey, we’re electronic health records too,” even though the reality is they don’t have a lot of presence in the electronic health records space.
Hospitals have gotten more involved in some of the practice EMR decisions more than a lot of people expected. What is it that they’re looking to accomplish?
It’s been very interesting because a few years ago, there were a lot of folks who were writing hospitals off. I think that hospitals — many hospitals — have been very strategic, have used the relaxation of Stark paired with these incentives as a way to say to physicians, “We will get connected to you and we will help supply the know-how, the technology, the hosting in some cases, and we’ll make it easy for you to adopt electronic health records. In many cases, we’ll provide additional funding to provide those electronic health records.”
So hospitals are playing an important strategic role, especially with smaller practices, as one way that electronic health records are going to get adopted.
Do you think Regional Extension Centers will have that same kind of impact in moving doctors along the EMR continuum?
I think no one’s exactly sure the impact of the Regional Extension Centers. We all hope that they accelerate adoption. We all hope they play a role in connecting physicians with solutions that work in providing support and training to those physician practices.
I think there’s some concern that putting a third party in between some of the users of the systems — the physicians and other caregivers — and the providers of the system, organizations like Allscripts and our competitors, may in fact, slow the process. I think there’s a lot of eyes focused on the Regional Extension Centers — exactly how they will operate and the role they will play.
We are very interested in being of assistance to them. We’re working with some of them right now. We’ve been fortunate to have been selected in some of the areas so far. So all of that is very good, relative to how those are operating. But I think it remains to be seen, the exact impact that they’re going to have, but we’re hopeful.
Would you say your biggest competitive pressure is aggressive competitors or lack of physician adoption?
It’s a good question because not too long ago, I spoke at an investment conference. One of our major competitors went right before me and they talked about a pause. The physicians were waiting to adopt to see how meaningful use came out and the like.
I came out afterwards and I said, “All we’re seeing is interest in acceleration.” And in fact, last quarter, we publically reported that our bookings — our sales number — was a 47% increase year-over-year. I think that indicates what we’re seeing, which is very, very strong interest and strong buying signals and strong buying.
We’re already seeing that. We don’t see that as a hurdle. Frankly, we see the same competitors that we always see, At the high end, typically Epic. In the mid-market, we see Quality Systems. In the smaller independent physician groups,less than ten, we see eClinicalWorks. Those are the three. Those are the kind of primary competitors in each of the three measurable market segments, if you will.
We’re seeing strong demand, strong interest, and we’re seeing that right now. We also see, as you’ve already mentioned, a lot of the larger hospital systems getting very actively involved in physician adoption and the acceleration of these systems. We think that’s very good and very healthy because that’s what’s going to help connect all of these systems together, which is very important.
Some of the U.K. financial analysts are opining that Misys should be getting out of the healthcare IT business to focus on their financial business. What would the impact be on Allscripts and its customers if, for some reason, they decided to do that?
Misys is a large shareholder, as you know. We stay focused on what’s happening in healthcare in the U.S. and we’ll let the U.K. folks speculate and analysts speculate.
The reality is we have the largest base of physicians in U.S. healthcare, almost one in three physicians in the United States, or over 160,000. We’re the largest player in practice management systems. We have the largest group of physician offices in the “less than 10” space. We’re the largest provider of electronic health records.
When you look at all of that, the reality is, we’re the market leader. We’re here and we’re going to keep executing. Who exactly owns which shares at what time has very little impact on how we’re running the day-to-day business.
I think that U.K. analysts speculating about the fact that the shares that Misys PLC as a publicly London-traded corporation owns in Allscripts had become very valuable. There’s some speculation that if they split up the company that you could get better shareholder return. That’s really analysts speculating.
No different than last week. I heard two rumors. One, that NextGen was being sold. Another one that Cerner was being sold. That’s speculation as well and I treat that all in the same way. We’ve got a business that’s growing very rapidly. We’ve got clients that we’ve got to satisfy. We’ve got the largest R&D investment in the industry. That’s what I spend my time on.
The Misys merger didn’t seem all that attractive when it was announced, but it looks smart now. Are there other acquisitions that would help round out your offerings?
We’ve said all along that we don’t need to acquire anything else to execute on our strategy and to be successful in the market. That said, we’ve also said that it’s clear that the industry is going to consolidate, that there are going to be opportunities, and fortunately we have a very strong balance sheet. We have very strong cash flow and revenues and we’ve got an increasingly strong management team. We’re going to be opportunistic.
But right now, again, our main focus — what we call ‘true north’ — is all about taking advantage of the stimulus. We’re at a very unique time here. We think this is the fastest transformation of a large sector of the U.S. economy in the history of the U.S. What we’re watching is this major sector that’s going to transform faster than any other sector in history, and Allscripts is positioned as the leader in the sector in leading that transformation. So that has to remain, and is, our focus.
That said; we’re going to continue as we have in the past to be opportunistic. When we did the merger, as you point out, people didn’t quite understand it. They think our competitors understood it because they kept saying, “Hey, this is going to fail.” But much to their dismay, we executed very strongly. We stayed focused. We executed against it and we have a much stronger company today, and the beneficiaries are our customers because they’re getting more products, more R&D, better execution, than ever before.
I think one good example is — I don’t have to tell you — in the past there were a lot of questions about our investment in our Version 11 Enterprise software, and we had some challenges. Anytime we do something really innovative, there’s some risk, and we had some challenges. The great news is just at the right time, we’ve moved past those challenges. Now we’re installing it faster than ever — 40% faster.
It’s interesting. There’s the competitors and other folks who like to focus on the past, but when you look at the numbers, it’s pretty astounding. In October, there were more than 24,000 physicians using Version 11 Enterprise software. That’s the equivalent of about 3½ million patients being touched. There were millions of prescriptions written and over 13 million orders. When you look at those kind of numbers and people say, “Oh, they’re having problems,” and this and that; that’s about the past. We’re very focused on the future.
Do you think, as a company, that was a valuable learning experience — the struggles with Version 11?
It’s always a valuable learning experience, but I think that the sign of a great company is to take risks, to provide innovative products, and if you have challenges, you work your way through them.
The great news is if you talk to some of our customers that experienced those issues, what they’ll tell you is — did they have problems? Yes, they did. Did they work through them? Yes, they did. Did you ever doubt that they would figure it out? And they say, “Nope, never doubted it.” Did they ever stop taking their calls? Did Glen ever stop picking up the phone when you called? The answer was no. We went head-on. We worked closely with our clients and we resolved them and we’re better for it.
If you name me a great company, a world-class company, I’ll tell you one or two areas where they went out, they tried something, and they may have had some challenges, but they worked through it and they’re stronger for it. You always learn from your mistakes if you’re good and you get stronger for it.
The issue is that no one ever doubted our resolve. No one ever doubted that we were going to get there, because unlike some of our competitors, this is our only business. This is what we live for. This is why you and I and others are here on Friday night, right? Because this isn’t just about a business, this is a passion. We want to transform healthcare and we want to lead that transformation.
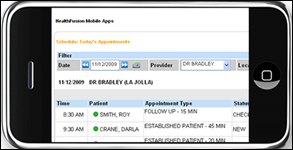
At the end of the day, software changes. The software we’re selling today, two years from now is going to be different. But when you look at innovation, when you look at just the innovation that we’ve introduced in the last year — software available on the iPhone. It’s available on BlackBerry, it’s available on Windows Mobile.
We have a leading kiosk. I was just at George Washington University Medical Faculty Associates. I was in their lobby with the CEO and some folks from the White House, and you put your hand in and it reads the veins in your hand. It takes your picture, scans your credit card, facilitates payment, patients are checking themselves in.
What was fascinating was that the CEO stood there with me and he said, “I want to show you something.” I said, “Well I’ve seen our kiosk there. That’s really cool.” He said, “No, no, no. Do you notice that there’s people waiting in line to use the kiosks and we have people — the normal check-in procedures — and they’re waiting and there’s empty desks?” And he says, “We need more kiosks.” But people are more comfortable and they like using the kiosk, and they feel more secure and we get more information from the kiosks then we get from the paper-based check-in process.
When you’re introducing this kind of innovation, along the way, are you going to have some hiccups? Of course you are. By the way, I always say to people who are implementing electronic health records, I tell them, “I can almost guarantee that you’re going to have some challenges if you do it right.” If you implement the system, not just to do what you were always doing, but to challenge some basic assumptions, to put some new processes in.
But I also tell them that no one in the industry is going to stick with you and be there to help you figure it out and optimize the use of this technology like Allscripts. So lesson learned for sure, but does that make us gun shy in the future? No, because there’s no one else in the industry that can do real-time clinical trials. There’s no one else in the industry that can provide the kind of connectivity and services that we’ll be able to provide. That’s in part because we are willing to go out there and take software that people like and upgrade it and go to the next level. There’s always some risk in that.
When you talk about the stimulus bill, what aspects of it do you think have changed since the original thoughts about how the money should be spent versus now?
The best thing about this is prior to passage, there was at least some school of thought that said we’re going to give every physician $15,000 if they don’t have an electronic health record. Fortunately, that was changed and the idea was that, look, just giving physicians money to buy one doesn’t get the taxpayer — who is the ultimate patient — doesn’t get them the benefit.
That’s where meaningful use came in. This was a very good bill because it said, not only do you have to buy it, but you’ve got to use it. You’ve got to see the benefit of it, and that’s really what’s going to help transform our healthcare system. So fundamentally, this is a very good idea.
Relative to meaningful use, we have been pushing very hard to say these standards ought to be tougher than they were in the past; and in some areas like interoperability, I’m not sure that we’ve been as aggressive as we should be. We are pushing to have some dates out there by which every system will have to talk to each other. The idea that in 18 months or 24 months, every system needs to pass messages, not only being able to send it, but receive it with the patient information.
Those kind of things ought to be required with a definitive date by which, if you don’t do it by that date, there’s no funding. We want to make sure this bill gets the taxpayer a return on investment because they are making a very big investment. If that means pushing the vendors a little harder, so be it.
That said, I think directionally this is very good. What we’re saying is we need privacy. We need security. But then we’re going on to say we need some clinical return on investment. We need the uploading to registries. We need the ability to write electronic prescriptions; and clinically, we need interoperability. Because what we can’t do is replace our paper silos of today with computer silos of tomorrow.
We need an interoperable system no different than the ATM networks that we use, no different than cellular networks. We have many different competitors, but they’re all using — they’re all connected to a network exchanging information; and of course, no different than the Internet. That’s the model that everyone ought to be forced to play in. We have some holdouts who are really not supporting this idea of full interoperability. So if I could change one thing, I would say we’ve got to much more aggressively push on interoperability.
Once the stimulus bill has encouraged the purchase of systems that are available today, how do we get to the next generation of systems and what are they going to look like?
Keep in mind — and this is not readily understood — what the bill actually says is each year, you’re going to have to affectively re-qualify. Each year, the standards are going to get tougher. That’s good news, and what that really says is that we have an opportunity to continue to push the vendors and the industry forward.
That said, I believe the biggest changes that we’re going to see are not necessarily in functionality. They will come in interoperability and connectivity. They will come in the ability to deliver real-time information to physicians, and they will come in ease of use.
In the future, I see a system that we ship, perhaps, through an ASP cloud-type system to a physician. He or she downloads that. There’s no training involved, it’s completely intuitive. Then when he or she sees the patient, there’s information provided to them that says, “Here’s best practices. Here’s the way this patient’s plan would like you to treat them. Here’s the medications. Here’s what they’re allergic to.” They get a whole information briefing just like a financial analyst or a stock trader would get on a stock before he or she would purchase it.
That requires a few things: very smart systems; very good connectivity; and a focus and an understanding that the healthcare system of the future is an information-based system. Healthcare, at the end of the day, is an information business. We have the best physicians in the world. We have the best medications in the world. We have the best medical technology in the world. What we need to do now is equip our physicians with the best information in the world to allow them to take advantage of all those tools. That’s what we haven’t done to date. That’s what I think this new world of healthcare will allow us to do. What we have to do is make sure we don’t squander that opportunity by setting our standards and setting our objectives too low.
That’s where we are today. We’re fortunate to have great products. We’ve moved past some of the challenges that we had in the past. I think everyone has concluded that the Misys merger, which is over a year old now and in one respect is old news, and in another way it’s old news because nobody’s really focused on it any more. But the good news is that gave us the tools and the footprint to compete in this new world of healthcare.
While we had some challenges with our Enterprise software, the good news is that the clients who are being installed today are very pleased with it. In fact, we just this past week had one of the largest go-lives that we’ve had with a client, with Sharp HealthCare out in California. They went live on the order entry phase of their project with hundreds of physician in a big bang, and it went unbelievably smoothly — so 350 physicians simultaneously live on order entry. The physician informaticist there noted that this go-live was flawless and the physicians loved the workflow, in part because they helped design it. The reality is a year and a half ago, I couldn’t have said that to you, so that’s what you’re seeing today.
That’s what we’re seeing with some of the great new expansions. We have North Shore-Long Island Jewish, a great example of a commitment to not only electronic health records and practice management — not only for their employee physicians, but for the entire community — and then a vision to connect all those electronic health records to 13 hospitals and to their entire home healthcare network. Now that’s pretty expansive vision. So kudos to the leadership shown by Mike Dowling and the whole North Shore-Long Island management team. We’re going to see a lot more of that.
Then we saw similar kinds of efforts going on in Hartford. Harford is built without any federal funding. They’ve essentially created an HIE that’s connecting a good part of the state now. It’s 20 hospitals the state’s top physician groups, Hartford Healthcare, St. Francis Medical Center, ProHealth Physicians, and I could go on and on. But these folks came together and said, “The time is now. Let’s get going.” They weren’t held back by, “Oh, there’s a problem with the software,” or anything like that. They’re making it happen real-time, so we’re pretty proud to be associated with folks like that.
Any final thoughts?
This is not an issue of technology any longer. This is an issue of leadership. The great healthcare organizations, whether they’re academic medical centers or integrated delivery networks, or whether they’re three-doc practices in Wilmette, Illinois or Tampa Bay, Florida; the fact that people are moving ahead and making this happen is really critically important.
The great news is that, especially as you move down into that smaller base to our Professional software, we have some pretty amazing customer data that 100% of our Professional EHR clients said their implementation — these were ones that were newly implemented in the last six months — said their implementation was within budget and cost. That’s a pretty amazing statistic, and those are the smaller offices. Those aren’t some of the largest ones. Then you fast-forward to some of the largest organizations and you look at the success we’re having at a place like UMass where again, great success. They’re rolling out, not only for their employee physicians, but also for their community.
One last point and this is this interoperability point. I can’t stress that enough. We have to get this system connected because what we want, ultimately, is a connected system of health. Not healthcare, but of health. To do that, again, we’ve got to get everyone working together. The great news is that places like Lahey Clinic in Massachusetts — leading organizations that are visionary. Or Columbia — we are connecting with competitors there. We’re connecting with Eclipsys. Out at Sharp, we’re connecting with Cerner. At many smaller practices, we’re working with our direct competitors there. So it can be done.
What customers have to do is suggest that it be done because we won’t have one system of healthcare. Healthcare networks in different areas look different. The independent physician is not going away. We just have to figure out within that, how we allow people to compete, to innovate, but to be connected. That’s really critical.










The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…