The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…
Joel Diamond 10/28/09
Yet More Controlled Medical Terminology
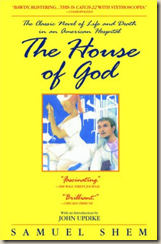
It’s been over 20 years since I read Samuel Shems’s irreverent and frighteningly realistic portrayal of medical training, House of God. It was unofficial required reading back then, and my fellow residents would quote lines as frequently as my teenage sons do from Judd Apatow movies today.
Shem referred to chronic, demented, elderly patients as GOMERS (Get Out of My Emergency Room), and Rule #1 was “GOMERS don’t die”. (Other rules were, “There is no body cavity that cannot be reached with a #14 needle and a good strong arm”, and “If the radiology resident and the Best Medical Student both see a lesion on the chest x-ray, there can be no lesion”.
I wonder how many current medical residents have read this book, and if so, does it still seem realistic? I trained near the tail-end of the days of legendary 36-hour shifts, unrestricted moonlighting, and unsupervised care at VA hospitals. The phrase “watch one, do one, teach one” was not a metaphor, it was a mandate.
Those days are gone. The tragic and famous Libby Zion case changed all that. For those who don’t remember, this young woman suffered and died as a result of a fatal medical error, allegedly due to unsupervised house staff weary from long hours. (Perhaps advanced decision support technology would have changed things … but I digress.) Her parents’ relentless publicity and appropriate legal proceedings brought much-needed reform to medical education by limiting work hours and requiring that attending physicians actually be present.
Despite this, many of us old-timers nostalgically look back to those days and sometimes wonder if current trainees lack the volume and richness of encounters that we find so invaluable in our current practices. Certainly, the gallows humor remains. So without further ado, more widely used medical terms that you won’t find in the books.
- Positive O Sign. Exhibited by an unresponsive, elderly patient. Characterized by their perpetually wide open mouth.
- Positive Q Sign. Similar to the O sign, but much more ominous, as their tongue is hanging out (thus resembling the letter “Q”).
- Throckmorton’s Sign. Experience clinicians would always point this out to naïve medical students. When looking at a male pelvic x-ray, the shadow of the man’s genitalia always points to the side of pathology (advanced research has confirmed its 50% predictive value).
- Emmerson Biggens Syndrome. Also used to to bewilder innocent students who could never find this condition in textbooks. Actually a misogynistic comment when looking at the chest x-ray of a well-endowed female patient (i.e. “‘em are some big ones”).
- Code Brown. As opposed to the better-known Code Blue, a true emergency where a patient has fecal incontinence, overpowering other disgusting odors usually present on wards.
While many of you laugh nervously at the apparent lack of compassion behind these references, remember that it often reflected an outlet for those dedicated clinicians on the front lines, toiling under unimaginable stress, which was frequently unappreciated and often futile.
Medical education has dramatically improved. More importantly, patients are rarely used anymore as mere training tools for inexperienced doctors-in-training. No doubt today’s tech-savvy residents (as well as increasingly complex patients) benefit from readily available medical information and computer-aided monitoring and support. Let’s not forget this as we design healthcare IT systems.

Joel Diamond, MD is chief medical officer at dbMotion, adjunct associate professor at the Department of Biomedical Informatics at the University of Pittsburgh, and a practicing physician at UPMC and of the Handelsman Family Practice in Pittsburgh, PA. He also blogs on interoperability.

At a code, first take your own pulse. The patient is the one with the disease. Buff and Turf. I still secretly categorize my ER docs as seives or walls.
One term that I believe I coined and that has become popular among the other residents in my residency program is “failure to die”, a twist on that nebulous ED admitting diagnosis of “failure to thrive” in an elderly, usually demented, and usually full-code patient who has no identifiable life-threatening acute illness but whom the ED doc just can’t justify sending back home or, more frequently, back to the nursing home from whence he came.