As rumored on HIStalk this weekend, Intuit announces plans to divest its health group, including the patient portal business it acquired from Medfusion in 2010 for $91 million. I wouldn’t be surprised if Intuit tried to find a buyer among its pool of resellers, which includes Allscripts, GE, and Greenway. I realize Allscripts recently purchased Jardogs’ patient portal technology, but Allscripts could still be a potential suitor given its large number of customers using the Intuit product.
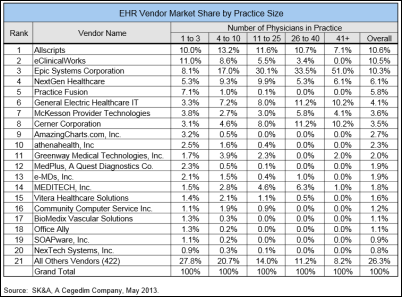
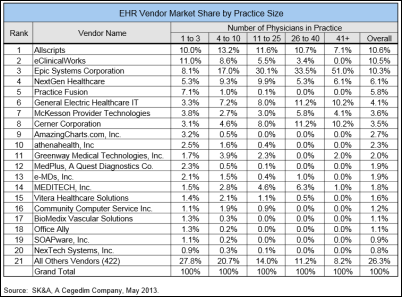
Allscripts, eClinicalWorks, and Epic lead all vendors in ambulatory EMR adoption, with just over 10 percent of the market each. Almost three-quarters of all practices using EMRs are supported by the top 20 vendors; over half of practices with more than 41 physicians use Epic.

CareCloud hires Paul Henry (ADP/AdvancedMD) as VP of small group sales.
Women’s Healthcare Associates (LA) selects the Vitera PM/EHR platform.

The ONC Beacon-EHR Vendor Affinity Group names Adele Allison, national director of government affairs for SuccessEHR, as co-chair, along with Chuck Tryon of MyHealth Access Network.
ZirMed announces that its first claims acceptance rate is averaging 98 percent or higher.
A Nebraska practice warns patients of the possibility of identity theft after a physician loses a thumb drive containing 2,125 patient records. The office says the lost records included patient demographic information but no social security numbers.
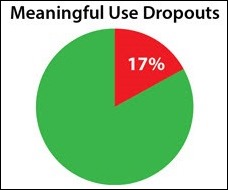
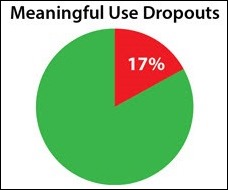
Thanks to SRSsoft CEO Evan Steele who did some number crunching and found that 17 percent of EPs earning an $18,000 EHR incentive in 2011 did not earn the $12,000 incentive in 2012. To earn the incentive in 2011, EPs had to demonstrate MU for 90 days. A full year’s demonstration was required for the follow-up year. As Evan states, “a 17 percent loss rate in any business is wholly unacceptable, and this failure does not portend well for the future of the EHR Incentive Program.”
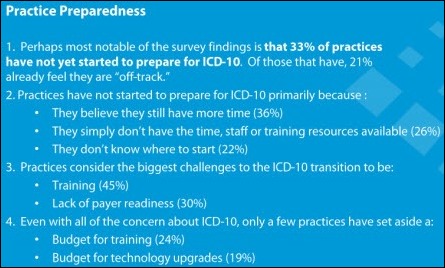
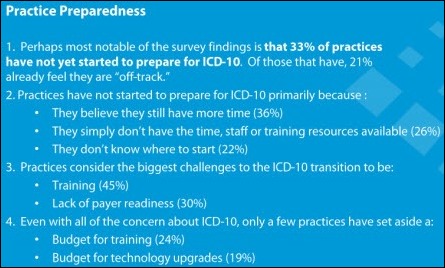
Porter Research looks at ICD-10 readiness among physician practices and finds that most are concerned with disruptions in cash flows when the new code set goes into effect. Of practices that have not yet started preparing for the transition, more than a third believe they have adequate time to prepare. The rest either don’t know where to begin or lack time, staff, or training resources.
Administrators at two Phoenix children’s clinics claim the use of scribes for EMR documentation has improved physician workflow, eliminated transcription costs, and improved revenue cycle. One orthopedic surgeons says the scribes “may have very well saved the clinic by helping with the implementation of the new EMR.”

E-mail Inga.

















Re: Walmart Health: Just had a great dental visit this morning, which was preceded by helpful reminders from Epic, and…