DOCtalk by Dr. Gregg 5/5/13
Dumbing Down and Smartening Up
Both sides of the healthcare provider/consumer “aisle” are talking about patient engagement and patient empowerment these days. The most interesting part of the recent momentum around these agenda items is that there doesn’t seem to be a whole lot of consensus on exactly what those two terms mean nor how they should be addressed.
On the patient empowerment side, people are talking about putting more emphasis on patient-centered care, making the patient the center of healthcare rather than having the provider or the institution or the insurance company or the technology vendor at the focal point. This seems like a no-brainer considering that the definition of “health” according to Merriam-Webster is “the condition of being sound in body, mind, or spirit.”
I’m not sure how anyone could see health and its care as anything other than a very personal, “patient-centered” issue. After all, body, mind, and spirit are unique to the individual. But, debates continue around who controls a person’s health data and how much access or input a person is allowed into their own care.
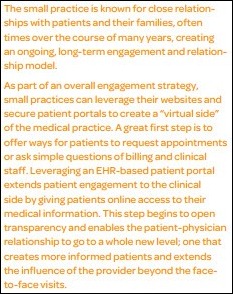
On the patient engagement issue, most people are focused on tech tools allowing providers to connect with patients and patients to connect with their health care data. This is important, but it seems to me that it’s not unlike the idea of giving everyone an iPad, but one with a DOS-like user interface. How “engaging” would that be? In other words, what good are patient engagement tools if the information and user experience (UX) aren’t “engaging?”
One thing seems clear: people on both sides are talking about making complex health information easier for non-medically trained people to understand. The impact of helping people to understand their health issues has been validated in numerous studies; when people understand their health issues (i.e., when their health literacy is higher), their health outcomes are better.
I’ve long been an advocate of simplifying medical information into “human-ese” to give patients the best chance of understanding complex medical information. I learned this years ago when making my own patient newsletters, back in the days when “desktop publishing” and “WYSIWYG” word processing were big buzzwords. (Yikes! Self-dating!!) Taking complicated health issues and trying to make them easy to understand and hopefully engaging for non-medically trained folks – and to do so for several such topics all on one side of a single piece of paper – was quite the challenge.
But, there are two sides to every aisle. The needs for understandable medical information in lay terms for lay people are quite different from the needs of providers for using medically complex jargon to communicate profession to professional.
The contentions of those who oppose “dumbing down” medical information have some valid arguments. If all of our medical documentation is to be available via patient portals and their ilk, providers fear that taking time to write all their notes in terms simple enough for patients to understand will take an ungodly amount of time. (And, providers’ time is precious enough as it is, what with all the coding and bullet points and mouse clicks and all!) Plus, some providers fear that the communication of professional concepts will be hampered, impeded even, if all of the complex medical terms used in patient records must be broken down into lay terms. (Imagine trying to sum up the tauopathy known as progressive supranuclear palsy – PSP, the cause of actor Dudley Moore’s death – into layman’s language when including it in a differential diagnosis!)
Me? I truly see both sides. I want my patients empowered; making things understandable for them helps that process. But, I also don’t want to see the simplicity of complicated conceptual discourse via sophisticated technical jargon fall prey to vocabulary Luddism.
It would seem that both sides of the aisle are correct. How we address this with a workable meet-in-the-middle approach is the real question. Bringing everyone onto a level health education and medical vocabulary playing field seems silly. Both of these so-called “smartening up” and “dumbing down” approaches have significant hurdles and/or negative impacts.
Thus, I propose a solution for which I’m far too uneducated (and, given my previous self-dating, likely far too old!):
- How about we set Watson, or a whole herd of smart humans and lesser computers, to the task of smartening up natural language processing to the point where I, as a doctor, can type any confoundedly complex medical lingo I want into a patient’s medical record and their patient portal spits out an NLP-derivation in regular old human-ese?
- Oh … and could we also task some UX experts to present that information in patient portals that are actually visually pleasing and truly engaging?
Just a dumb thought, from the trenches…
“I may be dumb, but I’m not stupid.” – Terry Bradshaw

Dr. Gregg Alexander, a grunt in the trenches pediatrician at Madison Pediatrics, is Chief Medical Officer for Health Nuts Media, an HIT and marketing consultant, and sits on the board of directors of the Ohio Health Information Partnership (OHIP).




















The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…