From the Consultant’s Corner 8/4/12
Business Intelligence: Shifting from Generating Reports to Creating a Body of Knowledge
Five years ago, the industry was buzzing about the concept of "business intelligence." Large, sophisticated healthcare organizations were gathering lots of data and running many reports in an attempt to answer key business questions. While this scattershot approach provided insight into certain aspects of the organizations, it did not help paint a comprehensive picture of enterprise-wide performance.
The reality is business intelligence isn’t about the amount of data or types of reports your organization generates. It involves creating a body of knowledge about your organization’s patients, care, and costs that you can use to drive process improvement, reflect compliance, and support decision making.
What I’ve noticed in talking with healthcare organizations around the country is that the art of leveraging business intelligence is not just for the large, sophisticated hospital or medical group any more. It is now a necessity for any organization that wants to survive and grow.
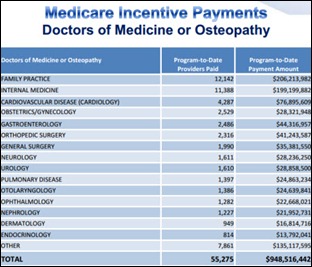
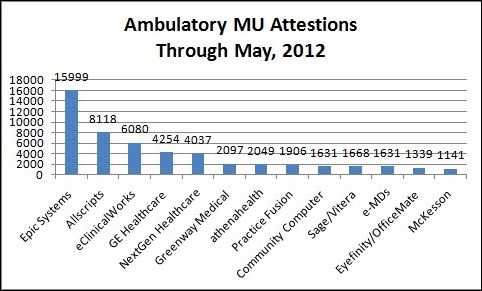
In fact, in the current age of data-driven healthcare policy—including Meaningful Use, patient-centered medical home, and healthcare effectiveness data and information set (HEDIS) requirements—organizations of all shapes and sizes need to use business intelligence to not only demonstrate compliance but, more importantly, to get paid.
A first step in the process of leveraging business intelligence is to take some time and clearly define what your organization’s approach to it will be. As part of this effort, I recommend creating a team of business intelligence consumers who can work together to determine what information is really needed and how your organization will use this key information.
The team’s membership should be diverse and include multiple perspectives, such as finance and accounting, clinical, and quality. The chief medical informatics officer (CMIO) should play a critical role on the team because he or she will bring both the business and the clinical perspectives to the table.
Note that the role of this group is not to figure out the technical aspects of gathering business intelligence. Leave that to the IT folks. This group needs to figure out the strategic goals for business intelligence and decide how the organization will use all the information it gathers. The ultimate purpose of business intelligence is to supply usable data that help develop better care for a better cost, so in my view, the team should be focused on things like how to develop a picture of overall performance, clinical quality, and patient satisfaction. BI should also reliably identify gaps in care and ways to improve revenue cycle efficiency.
I would caution you when taking this strategic look to consider not just what your organization needs now, but also what it will need five years down the road. As I mentioned earlier, many healthcare organizations used to take a more limited view of business intelligence and focused their attention on generating volumes of reports. Now these organizations are replacing many of the systems they purchased five years ago because they don’t have the bandwidth and capability to do what is necessary to meet current information needs. Your organization can avoid making this same mistake by focusing on the future, so that five years from now, you are optimizing solutions for business intelligence not replacing them.
Kyle Swarts is regional vice president for Culbert Healthcare Solutions.














Re: Walmart Health: Just had a great dental visit this morning, which was preceded by helpful reminders from Epic, and…