News 3/19/15
Top News
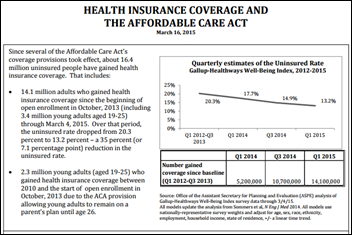
HHS reports that 16.4 million uninsured adults have gained insurance coverage since the implementation of the ACA.
Webinars

March 31 (Tuesday) 1:00 ET. “Best Practices for Increasing Patient Collections.” Sponsored by MedData. Presenter: Jason Bird, director of client operations, MedData. Healthcare is perhaps the last major industry where the consumer does not generally have access to what they owe and how they can pay for their services. Collecting from patients is estimated to cost up to four times more than collecting from payers and patient pay responsibility is projected to climb to 50 percent of the healthcare dollar by the end of the decade. Learn how creating a consumer-focused culture, one that emphasizes patient satisfaction over collections, can streamline your revenue cycle process and directly impact your bottom line.
Acquisitions, Funding, Business, and Stock

IBM and Twitter launch developer tools and cloud-based data analysis services that mine Twitter data five months after announcing their non-exclusive partnership. The data services run on IBM’s Watson technology and its BigInsights version of Hadoop. The developer tools will enable users to create tools that pull in Twitter data, a concept that has already provided itself useful in the area of population health.
![]()
Patient relationship management platform company Conversa Health closes a $2.5 million seed round with a group of unnamed healthcare angel investors.

Electronic Health Network accepts $200,000 from the SCRA Technology Ventures SC Launch program, which the health information exchange company joined in June 2014.

Zobreus Medical Corp. takes preorders for its Patient-Oriented Electronic Medical Record via Kickstarter at no cost aside from a one-time pledge. The company is looking to raise $50,000 by April 16.
Diabetes management app vendor Glooko raises $16.5 million in a Series B round.
Seattle-area Premera Blue Cross discovers that hackers have had access to the demographic, clinical, and claims information of 11 million people going back to May 2014. The FBI is investigating.
Announcements and Implementations
Migrant Health Center (PR) selects the eClinicalWorks EHR for implementation at its eight locations.
Genesis Medical Associates (PA) implements Treatspace’s interface tool for patient referrals to medical specialists. GMA formed the Keystone Clinical Partners ACO with nearby Preferred Primary Care Physicians in January, and no doubt hopes the new technology will help it drive down communication costs.

HealthPoint (WA) implements IOD’s Prism Connect Provider communications tool at its 13 clinics.
Telemedicine
The California Skin Institute partners with Iagnosis to launch teledermatology services for its patients. The practice, the largest of its kind in the state, also hopes to offer the new Derm On Call service to employers in the area.
The State of Idaho comes one step closer to passing telemedicine legislation after approval in both the House and Senate. Now awaiting the governor’s signature, the proposed bill would give the state’s licensing boards the task of setting their own rules and oversight on what medical services could be accessed via telemedicine.
Botswana is delivering broadband and telemedicine services to remote areas via unassigned TV band frequencies.
Government and Politics

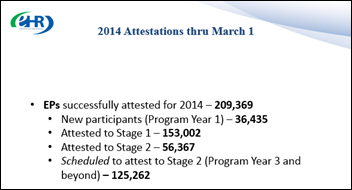
Lawmakers explore EHR adoption progress during a Senate Health, Education, Labor and Pensions Committee hearing, paying particular attention to the financial burden felt by many small practices struggling to keep up with Meaningful Use. AAFP President Robert Wergin, MD told the committee he wants to see Congress delay MU penalties for non-attesting physicians until interoperability is achieved.
CMS releases its physician referral data sets.
The House is finalizing a permanent SGR Medicare payment fix at a cost of $200 billion over 10 years, with taxpayers paying $140 billion and high-income seniors paying $60 billion in new Medicare costs.
The Obama administration achieves the dubious distinction of again setting a record for censoring government files or denying access to them last year under the U.S. Freedom of Information Act. HHS, however, was lauded for disclosing data about the Ebola outbreak and immigrant children caught illegally crossing U.S. borders.
People

Ebola survivor Rick Sacra, MD is named Family Physician of the Year by the Massachusetts Academy of Family Physicians.

Larry Ponemon (The Ponemon Institute) joins the advisory board of Immune-Secure, an Independent Security Evaluators-sponsored research study on security improvements in healthcare.
Research and Innovation
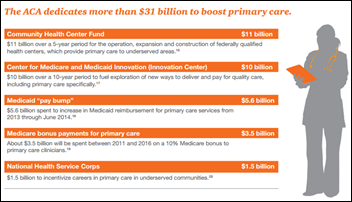
A PwC reports on the impact the Affordable Care Act has had on the healthcare industry five years after its passage, identifying primary care as the fulcrum between expanding insurance coverage and encouraging alternative payment models for care delivery. It also concludes that, while the ACA helped to kick start telemedicine services within physician practices, the use of virtual consultations will need to become more widespread if physicians hope to remain competitive in the new world of value-based service.
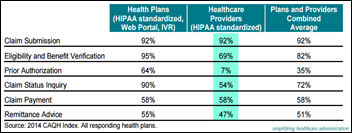
The Council for Affordable Quality Healthcare finds that transitioning from manual to electronic processes for claims submission, status inquiry, and payment; plus eligibility and benefit verification, prior authorization, and remittance advice could save healthcare providers and payers over $8 million a year. While not as sexy as digital health, these areas seem ripe for startup opportunity.
A survey of 500 healthcare professionals finds that 46 percent plan to introduce mobile apps into their practices within the next five years. A similar percentage believes apps will increase the efficiency of patient treatment. I’d like to see numbers on how these physicians plan to incorporate this new data into their daily workflows and EHRs, not to mention how they foresee being reimbursed for the time it takes to digest the data.
Other

Interior Design magazine profiles the life and passing of iconic architect and consumer goods designer Michael Graves. I was not aware that he put his unique spin on walking sticks, signage for the visually impaired, and wheelchairs.
Sponsor Updates
- PerfectServe posts “Real-time healthcare: Preventing the need for immediacy from eroding quality.”
- Culbert Healthcare Solutions will exhibit at AMGA 2015 Annual Conference March 24-26 in Las Vegas.
Contacts
Jennifer, Mr. H, Lorre, Dr. Jayne, Dr. Gregg, Lt. Dan
More news: HIStalk, HIStalk Connect.
Get HIStalk Practice updates.
Contact us online.






































The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…