News 12/1/11
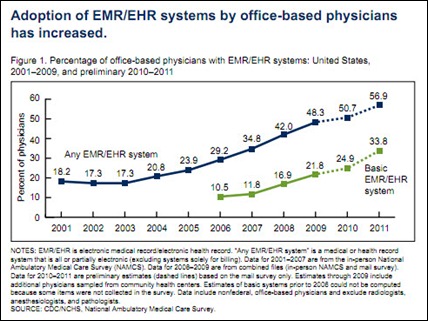
CMS extends the deadline for meeting Stage 2 Meaningful Use for hospitals and EPs that qualify for Stage 1 MU in 2011. In order to “make it easier to adopt health IT,” CMS says it will give all providers – those qualifying for Stage 1 in 2011 and in 2012 – until 2014 to achieve Stage 2 requirements. In the same press release, CMS also mentions a recent CDC report that estimates that the percentage of physicians who have adopted EHR in their practices has grown from 17% to 34% between 2008 and 2011. In addition, 50,000 HIT jobs have been created since the enactment of the HITECH act.
Other key findings from the above-mentioned CDC report, based on the National Ambulatory Medical Care Survey:
- 57% of office-based physicians use EMRs of any type.
- Provider usage rates range from 40% in Louisiana to 84% in North Dakota
- 52% of physicians surveyed in 2011 say they will apply for MU incentives, which is up from 41% in 2010.
Mountain Medical Physician Specialists (UT) chooses the Medicalis Enterprise Worklist platform to balance imaging volume across its 65 physicians and 15 reading sites.
The Detroit Medical Center PHO teams with the AMA’s Amgine subsidiary to give physician members access to AMA ePrescribe and the DocSite registry.
Cardiology Associates of North Mississippi adopts Emerge Clinical Solutions’ decision cardiology software, which is integrated with the practice’s GE Centricity PM system.
Navicure adds the 60-physician Family Health Services Minnesota and Pine Rest Christian Mental Health (MI) to its client roster. Navicure was also included on Deloitte’s Technology Fast 500 list for the fifth consecutive year.
The 30-radiologist Physicians Imaging Center of Florida contracts with Atlantic Health Management Solutions for billing services.
Medical Transcription eXpress signs with MD-IT to resell the MD-IT platform and EMR.
Memorial Healthcare System (FL) selects Meditab/SuiteMed as a vendor option for its EHR Donation Program. Affiliated MHS physicians will have the option to implement the Intelligent Medical Software EHR in connection with the Atlantic Coast HIE.
HealthSaaS and DocLogic collaborate to deliver health monitoring directly into live online encounters between physicians and patients. The companies will integrate HealthSaaS’s biometric and mobile applications with DocLogic’s telemedicine technology to improve remote patient monitoring. Captured data can then be sent electronically to physicians’ EHRs.
West Bay Orthopaedic Medical Group (CA) contracts for the ChartLogic EHR suite. In the same press release, ChartLogic says that more than 25 of its clients have qualified for Meaningful Use. I am not sure what percentage of ChartLogic’s total client base that represents, although the ChartLogic Website says “thousands” of practices use their EHR.
St. Jude Heritage Medical Group (CA) selects MediRevv to provide insurance backlog liquidation support and resolution services for its 150-doctor organization.

















The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…