News 9/30/10
From: Matt “Re: imedcenter. I noticed that you picked up the article about our clinic. What we are doing is extremely time consuming to invent from the ground u/p, especially for primary care type offices like ours. We really feel that the systems we put in place allow the patient to feel the personality of the old days of the home visit, while allow the physician to survive in the brutal primary care market.” When imedcenter of Danbury opens its doors this week, it will be totally paperless. I checked out their website and noticed that their HIT setup is not the only thing differentiates them from the masses: imedcenter providers are a unique combination of traditional MDs, naturopathic physicians, chiropractors, therapeutic massage therapists, and nutritionists.
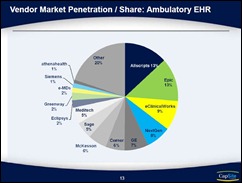
From: NoKlass “Re: KLAS and ambulatory solutions. What’s being ignored is the difference between enterprise systems that work in hospitals, and EMRs that work in ambulatory medical practices. Also missing is a distinction between EMRs that cater to specialists versus primary care.” Well said. On the other hand, if there are too many categories I can envision a whole other set of issues, not to mention plenty of criticism from vendors who are benefiting from the status quo.
The big Xconomy Exchange with eClinicalWorks’ Girish Navani and athenahealth’s Jonathan Bush is/was Wednesday. A reader sent in this stealth picture with promise of more details to follow.
Daily text messages reminding dermatology patients to take their medication significantly improve patient adherence, self-care behaviors, and quality of life, according to a Center for Connected Health study.
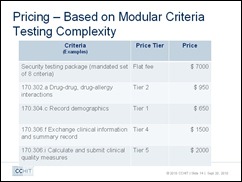
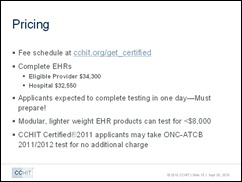
Also dermatology-related: dermatology-specific certification, such as the one CCHIT offers, will likely not sway EHR-resistant dermatologists to invest in a system. I’m sure one reason many dermatologists avoid adopting EHRs is because of their high patient volume: they don’t believe there’s time to document electronically and still see 40+ patients a day. In addition, ARRA won’t incent too many physicians to adopt EHR since the meaningful use measures are less relevant in dermatology.
A whopping 70% of medical students say that having an EHR is a very important factor in deciding where they will practice medicine (could the rest be considering dermatology?) Additionally, medical students love smartphone devices, particularly iPhones or iPod touches: 70% are Apple fans, followed by BlackBerry and Android devices.
Phreesia completes a $20 million Series D round of funding. Just this week, someone suggested I check out Phreesia, a company that has developed a patient check-in system that also verifies insurance eligibility, calculates the patient-responsible amount, and collects the money with a credit card swipe. Patients are handed a “PhreesiaPad” tablet device, take a seat in the waiting room, and complete all the check-up and payment tasks before being seen. The product is timely since more practices are attempting to collect the full patient-responsible money up front, rather than wait until insurance pays. What differentiates Phreesia from similar products is that the “collection” task is performed by the tablet and not the office staff, most of whom rather ask Mrs. Smith about her new grandbaby than break the news about a new payment procedure.
RCM-provider ZirMed achieves Phase I certification from the CAQH CORE, which means the company has proven its ability to provide real-time access to key eligibility and benefits data.
Western Maryland Health Systems selects Dell and eClinicalWorks as the hosted subscription-based EMR/PM solution for its 150 affiliated and 26 employed physicians. Dell will provide both the hardware and software support through its ProSupport EMR helpdesk.
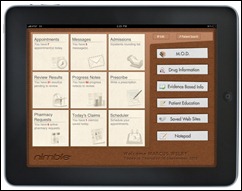
ClearPractice announces the release of Nimble, an EHR designed specifically for the iPad. I’m kind of wondering why, if you are going to run your software on a device with amazing graphical capabilities like the iPad, would you develop your software with a brown background. Anyway, the first 500 physicians to subscribe to ClearPractice’s Practice Edition EMR get a free iPad.
Blue Shield of California commits $24.8 million in 2010 payments to reward medical groups and IPAs that meet pay-for-performance objectives for clinical care, patient experience, and HIT adoption.
Coming to a mobile device near you: mobilePDR. Physicians Interactive Holdings and PDR Network are offering a mobile, digital version of the Physician’s Desk Reference. mobilePDR is available for free for full-time practicing physicians via PHI’s Skyscape mobile channel. Details here.














The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…