News 4/15/14
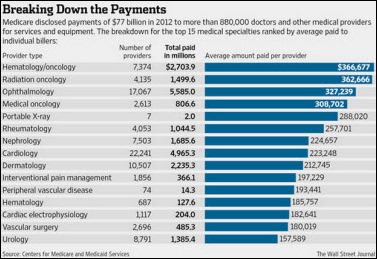
AAFP President Reid Blackwelder, MD offers an interesting spin to last week’s disclosure of Medicare payment data. Blackwelder notes that while the release may make some family physicians feel threatened, he points out that the “action taken by CMS will provide a great opportunity for the Academy to highlight the complexity of care that family physicians provide.” Blackwelder likely hopes the payment details will positively impact family physicians’ bottom lines, noting that the data reflects the disparity in compensation between specialists and family physicians, who “are near the bottom of the list in terms of payment.”
Meanwhile, the AMA emphasizes that CMS released “raw data with little context and considerable limitations” and offers some points of clarification to help physicians answer questions from inquiring patients. Key points include:
- Medicare payments don’t equate to a physician’s personal income. Physicians also have practice overhead and receive payments from other sources.
- The released data may be not include all services performed, could contain errors, and could include figures related to services rendered by residents or other providers.
- Claims data does not provide implicit details on outcomes.
Finally, let’s just hope the financial winners in all this are not the lawyers specializing in healthcare fraud cases. Not surprisingly, so-called whistleblower attorneys pounced on the data in hopes of expanding existing cases against providers and pharma companies and in search of leads for potential new lawsuits. I see a flood of late night commercials in the works urging medical billers to call a special toll-free number to report employers’ billings that might to be out of line with the rest of the industry.
Sermo reports that its online community has grown to 260,000 US physicians, which represents a 30 percent increase since October, 2013.
The 260-provider Phoebe Physician Group (GA) selects athenahealth for EHR/PM and care coordination.
Shenandoah Medical Center (IA) will deploy Allscripts Sunrise solutions, including Allscripts Sunrise Ambulatory Care.
DrChrono raises an additional $2.69 million in convertible debt funding, giving it overall funding of $6.77 million. The company offers a free EHR platform and says 60,000 physicians are “signed up” to use their program. I assume that number includes me after I took about 30 seconds to register my “family practice.” The website says that DrChrono is Stage 1 certified, however Stage 2 certification is not mentioned. Regardless of my doubts, investors seemed to have found their story compelling enough to pony up additional funds.
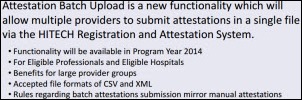
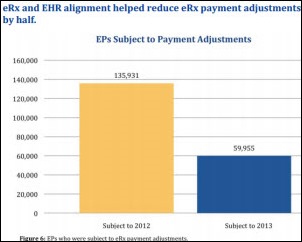
CMS offers guidance on how providers can take advantage of the new Attestation Batch Upload option, which allows multiple EPs (and hospitals) to submit attestations in a single file through CMS. Incentive payments are provided to individual providers and not to medical groups or hospital systems, even if attestation is submitted in batches.
Here’s a different twist to the standard privacy breach. A former administrative assistant at a Tennessee urology practices sends a competing practice the names and addresses of 1,114 patients so the competitor could solicit business. No data commonly used for identity theft was provided, nor any clinical information. So far no word on possible charges filed against the terminated employee, nor the competing practice.
The Boston Business Journal names athenahealth the top publically traded Massachusetts software company with the largest market capitalization at $5.5 billion. Nuance Communications was a close second with a market cap of $5.2 billion.
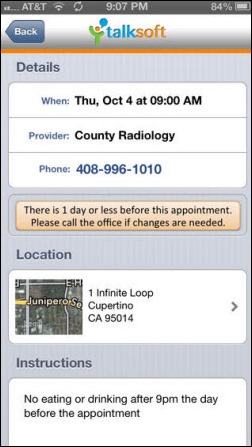
Talksoft Corporation makes its appointment reminder app Talksoft Connect available for Android devices. The app allows patients to confirm or request a reschedule, alerts patients of a payment due, and offers automatic entry and alarms on a device’s calendar.
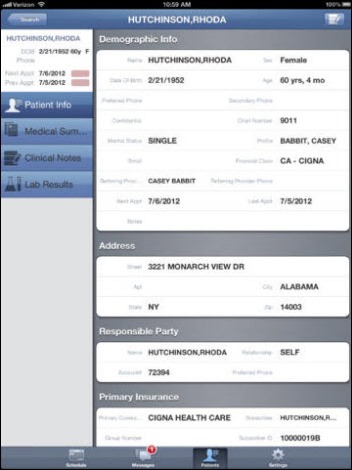
AdvancedMD introduces the 1.5 version of its iPad release that includes image capturing within notes, patient search enhancements, a refreshed interface for iOS 7, and faster messaging capabilities.
A Texas family physician finds professional satisfaction after ditching insurance and charging his largely uninsured patient base a flat $50 fee per visit. The “direct primary care” model isn’t new but may find new popularity from physicians opting to avoid administrative overhead and billing hassles. Unlike the concierge model where doctors charge higher annual fees and spend more time with fewer patients, Laredo physician Gustavo Villarreal, MD (above, in front of his paper charts) sees 40 to 60 patients a day and says the change has made him feel like he’s a doctor again.
Email Inga.
















The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…