HIT Vendor Executives on Expectations and Plans for 2014 – Part One of a Series
We asked several vendor executives a series of three questions related to their expectations and plans for 2014.
What will be the biggest challenges facing physicians and physician practices in 2014 and how will these trends impact their use of technology?
Raul Villar, president, ADP AdvancedMD
In 2014, physicians in private practice will be challenged with mastering Meaningful Use, weathering the implementation of ACA within the industry and its impact on patient population and reimbursements, preparing for the switch to ICD-10, and juggling everyday issues and challenges to ensure today’s claims will get paid in a reasonable amount of time.
Compliance complexity in each of these areas dictates the use of automation solutions so physicians can focus on patients. This is especially acute in smaller independent practices that do not have the staff or IT departments to manage compliance. In this environment it will be critical for practices to work with technologies and vendors with compliance upgrades included in their products and processes vs. those requiring the practice to shoulder the responsibility of upgrading technology to remain compliant.
Under ICD-10, the benefits of fully integrated PM and EHR solutions will be dramatic as practices are required to produce more complex charting and coding in their EHRs. Having ICD-10 compliant charts flow directly into billing in fully integrated systems will reduce errors and rework.
Jim Hewitt, VP of solutions development, Allscripts
2014 is going to be a very busy year for physicians and their practices. The biggest challenge for most practices will be managing their system upgrades for MU2 and ICD10. On top of that, they will continue to move to a value-based care model which will be a major operational and financial shift for them. They’re going to need technology to help them manage their risk-based contracts as well as proactively manage their populations.
The other big challenge for physician practices is implementing a patient engagement strategy to meet MU2 requirements. Not only do they need to implement a solution, they need to engage patient populations to use the technology.
Todd Rothenhaus, MD, CMO, athenahealth
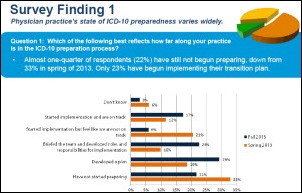
You can’t think of 2014 challenges in health care without thinking of ICD-10. Our annual Physician Sentiment Index survey, completed in 2013, showed physicians’ confidence in their practice’s ability to transition to ICD-10 is extremely low with only 8% saying they were “very confident” that the transition would happen smoothly. ICD-10, for too many, will be difficult and another massive “must do,” that needs to get done – in addition to Meaningful Use stage 2, and perhaps most overwhelming, smack in the middle as physicians and practices work to navigate and understand changing reimbursement models and their associated expectations – most importantly the ability to coordinate care.
I think in 2014 we’ll also see a massive EHR shopping spree and replacement trend that will be driven by significant failings of vendors who didn’t adequately support things like ICD-10, Meaningful Use, and aren’t building network-based open platforms to enable their clients (physicians/health systems) to truly coordinate care across the continuum. The tides in health care are changing and so will the technology that is deemed necessary to survive, let alone thrive.
Albert Santalo, CEO, CareCloud
This is always top of mind for us, so it’s something we’re constantly asking physicians about. Just a few months back, thePractice Profitability Index (PPI) – which surveyed more than 5,000 physician participants regarding issues impacting the financial and operational status of their practices – found that three of the top four issues negatively affecting profitability for all physicians stemmed from healthcare reform, led by declining reimbursements (65 percent), rising costs (57 percent), Affordable Care Act-related requirements (48 percent) and coding and documentation changes, including ICD-10 (44 percent).
Stephen Ober, MD, chief medical officer, Emdeon
The biggest challenges facing physicians and physician practices in 2014 revolve around patient engagement in two themes:
1) continued interaction with patients after they leave the provider’s office, and
2) how to assure that the practice is meeting the payer performance criteria they signed up for earlier this year. Providers have to engage patients through technologies (portals, cell texts, etc.) to continue the relationship after the acute encounter. From a clinical performance standpoint, practicing providers have to understand the metrics that the payers are evaluating them against. Some provider groups fail to push these criteria down to the practicing clinician.
Patrick Hall, EVP of business development, e-MDs
ICD-10 compliance will present a unique challenge. Practices will need to invest not just in technology, but also the time and effort to learn the new coding system and, depending upon how their vendors/partners deal with the change, potentially modify existing systems and workflows to make the transition.
Many physicians will also need to adapt to an increasingly “open” environment with respect to exposing information to patients through portals and other tools. Patients are starting to expect this and so physicians and their staff will need appropriate protocols in place with respect not to whether information is shared, but how and when in the clinical information cycle.
Tee Green, CEO, Greenway Medical Technologies
There are three fundamental trends that will create both challenges and opportunities for physicians in 2014 while impacting their use of technology. The first is the electronification of healthcare, which will continue to progress rapidly in the ramp-up to ICD-10 compliance, meaningful use Stage 2 and other industry changes. Electronic health records are only one component of this trend, and it’s evolving to include access to real-time clinical insight that is available inside and outside of healthcare settings.
A second trend is consumerism. Consumer expectations now drive fundamental changes to the way healthcare is purchased and delivered in our country. As individuals become increasingly responsible for a greater share of their healthcare costs, they will no longer accept inefficiency and redundancy in care. They also have high expectations around convenience. As a result, physicians must be more transparent about costs and quality, while making it easier for patients to engage in their care.
Another trend is an increased focus on improving population health as physician groups take on greater risk and accountability through value-based medicine payment models. Technology that can give physicians the ability to monitor clinical and financial metrics, while identifying and managing at-risk patients, will be essential to addressing this challenge.
Tom Giannulli, MD, CMIO, Kareo
2014 is going to be a year of big changes for healthcare providers. The biggest challenges are going to be ICD-10, ACA, Meaningful Use, and the ongoing shift to more patient-centered care. Each one of these comes with its own unique issues, and the use of technology will be invaluable all the way around. It’s a given that you need an EHR for MU and a good billing system for ICD-10. The gray areas are the ACA and the growing movement to more patient-centered care. We still don’t know exactly how these things will play out so a practice needs to prepare for the unexpected. To do that you need to optimize your practice with the most seamlessly integrated and robust practice management, billing, and EHR solution you can find.
Nick van Terheyden, MD, CMIO, Nuance
The ICD-10 transition will impact providers and their organizations the most in the year ahead. Under the new coding requirements, physicians will be mandated to document in a more detailed and complete way in order to justify the same care they’ve been delivering for years. From a clinician’s perspective, the transition will pull their focus away from the patient and force them to devote even more of their time and attention to technology, documentation and administrative tasks. Added to the challenges physicians are already facing with EHRs, ICD-10 will create a perfect storm. As a result, we’re going to see an increasing demand for technologies that re-connect physicians with patients, and bring them back to focusing on the art of medicine, while still enabling them to meet the new regulatory and reimbursement standards.
Irtaza Barlas, director of software engineering NueMD
Biggest challenges facing physicians:
a) Given that the year 2014 may go down as the ‘the mandate year’, physicians in many specialties will be enrolling new patients. New insurance plans for new and existing patients will continue to be created that will make the medical billing potentially more complex.
b) Since 1979, physicians have been happily using the ICD-9 coding to classify diseases. With ICD-10 being introduced later this year, a major learning curve awaits the back office.
c) With more interconnectivity will come more headaches to manage patient data in a secured manner.
Chip Hart, director of strategic marketing/sales director, Physician’s Computer Company
As a practical matter, it’ll be ICD-10 and SNOMED. The former is going to kill insurance company payments for an unknown period of time, which is a giant cash flow issue. The latter is going to change the EHR flow for many groups as their vendors race to comply with Stage 2 with a lot of time to get used to it.
Frankly, other obligatory demands will also be a problem – particularly from HIEs and the need to integrate with some newly (read: poorly) formed ACO. I really hope that last prediction is wrong.
Michael Brozino, president and CEO, simplifyMD
The impact of the Patient Protection and Affordable Care Act (PPACA), the transition to ICD-10, Meaningful Use Stage 2 and emerging value-based payment models are all challenges physicians and practices will face this year. These changes, along with increased clinical data demands from payers, can distract physicians from their core mission of caring for their patients while maintaining a profitable practice. To succeed in this environment, physicians need a flexible EHR and PM system that helps them work more efficiently so they can improve productivity while monitoring their quality of care metrics.
In 2014, many practices will be replacing their current EHR systems with ONC-certified software that supports their preferred workflow and improves productivity while complying with the demands of the PPACA, transition to ICD-10 and attestation of Meaningful Use Stage 2. These replacement systems will need to be flexible and customizable enough to evolve with the practice allowing physicians the ability to capture additional data for clinical quality improvement initiatives or financial data analysis.



























The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…