News 12/18/12
Epic wins big in the Physician Practice Solutions categories in the 2012 Best in KLAS Awards, taking the top spot in the “Over 75 physicians” categories for both EMR and PM and for the “11-75 physicians” EMR category. AthenaClinicals was the leader in the 1-10 physician EMR segment and for PM in both the 11-75 and 1-10 physicians segments. Other observations: a) Allscripts, McKesson, Vitera, and GE populated the bottom spots on the EMR rankings; b) Greenway and eClinicalworks had solid EMR rankings; c) NextGen, GE, Greenway, and e-MDs scored well in the PM segments; and d) Vitera, Allscripts, eClinicalWorks, and McKesson had the lowest spots in the PM categories.
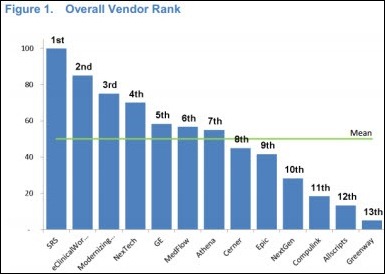
A reader forwarded me another user satisfaction survey produced by University Survey. The report looked at ambulatory EMRs and included responses from 1,051 specialists (ophthalmologists, dermatologists, and cardiologists). The top-rated products were SRS and eClinicalWorks, while Allscripts and Greenway were ranked last. Specialists have different EMR requirements and their product preferences aren’t necessarily the same as primary care providers, but I am a little suspect of the quality of data, primarily because (a) University Survey would not respond to my direct question about whether or not a vendor or some other entity paid for the survey to be conducted, and (b) the report offers no details on the survey methodology. My opinion: KLAS, University Survey, Black Book, and similar surveys provide interesting data points, but should never be the sole consideration when making a buying decision.
The world seems like a troubling place at the moment, making it a perfect time to add a bit of levity to your day. Take a minute to read Joel Diamond’s Year in Review post, which provides a tongue-in-cheek look at the most compelling HIT news events for 2012.
American Family Care, which has 34 locations across Alabama, Tennessee, and Georgia, completes its implementation of DocuTAP’s EMR and PM products.
The 370-physician Kelsey-Seybold Clinic (TX) becomes the first healthcare organization to earn NCQA accreditation as an ACO.
Vitera Healthcare announces the general release of Live Chat, which provides customers with immediate online access to Vitera customer support.
Assuming you are reading this post on a desktop or laptop and not a mobile device, you have likely noticed our brand new HIStalk Practice Web page format and logo. We refreshed HIStalk Mobile (now known as HIStalk Connect) a couple of weeks ago and HIStalk’s transition is coming soon. A big thank you to the folks at Dodge Communications for the providing us with the snappy logo designs. We really hope you like the new look.














The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…