News 10/11/11
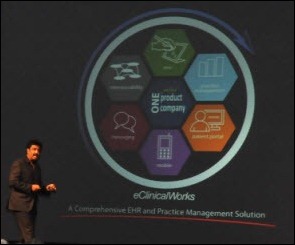
eClinicalWorks takes the top stop on the Worcester Business Journal’s list of top-growing private regional companies for 2011. The publication profiles eClinicalWorks, which has grown from $1 million in revenue in 2003 and should hit $200 million for 2011. CEO Girish Navani says that eClinicalWorks has added 350 jobs and over the last year and predicts adding another 200 people in the near future.
The CEO of Pulse Systems says his company is preparing to release an iPhone app, a self-service patient kiosk, and an online patient portal.
Healthcare employment continues to rise with ambulatory health services adding 26,000 jobs in September and hospitals adding 13,300.
The 15-physician Primary Health Care Marshalltown Clinic (IA) goes live on GE Centricity EMR.
EMRapproved.com, a online EMR consulting resource, launches Tech Savvy Doc Directory, which is purported to be the “first-of-its-kind nationwide listing of physicians who offer EMR and communication tools in their practices.” The idea is that patients can enter their zip code and a specialty and find all the physicians in the area that use EMR. Sounds nifty but when I test-drove it the results were less than impressive (two physicians total in my zip code, which I know is way off.) I wonder how they intend to identify whether a doctors uses EMR? More importantly, will the use of EMR really influence a patient to select one provider over another?
HIE provider Sandlot partners with EHR provider TactusMD to provide a package solution for pediatric healthcare communities that don’t have an integrated EHR and HIE solution.
Medical residents are the subject of intense recruiting activity, with 78% being contacted more than 50 times about job opportunities at hospitals or physician groups. A third of the residents say they’d prefer to work for a hospital, while 28% claim a preference for working in a physician group as a partner.
More bleak news on the effect of rising healthcare costs: Americans are spending more on insurance premiums, co-pays, and deductibles, leaving them with less money to spend on out of pocket health services. As a results, patients are putting off doctors’ visits or medical procedures, declining tests, and ordering less expensive drugs.
athenahealth CEO Jonathan Bush tells an HIT Policy Committee Meaningful Use Workgroup that physicians should be required to submit actual performance data to CMS, rather than simply attest they have met Meaningful Use guidelines:
“To increase the integrity of the program and leverage data that should already be maintained in EHRs, CMS should aggressively pursue a registry-based submission process for provider attestation. Until Meaningful Use performance data can be electronically submitted from a provider’s EHR, attestation unnecessarily remains a subjective and qualitative measure of success–forcing undue stress on providers, creating the need for stringent and costly after-the-fact audits, and underutilizing the capabilities of EHRs.”
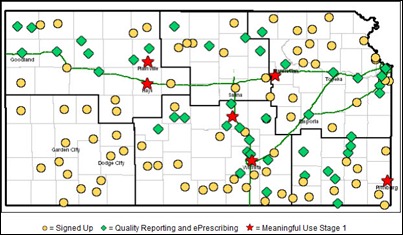
The Kansas Foundation for Medical Care reports that its REC is now working with 1,002 physicians and practitioners, including 911 primary care providers and 81 specialists.

















The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…