A Quick Peek at … athenaClinicals
Readers often ask us for our insights on various HIT products. Though we would like think we are experts in all things HIT, the truth is there are far too many applications out there for us to provide in-depth opinions on them all.
However, in our constant quest for knowledge, we decided it would be fun to take a quick peek at a few products. The folks at athenahealth were gracious enough to serve as the guinea pigs for this first review and did a demo for us. Our instructions to athenahealth were to provide an overview of their athenaClinicals product in about an hour’s time. We did not advise them in advance what specific areas we would be evaluating (which in hindsight, perhaps we should have). Because of time constraints, we did not have a chance to go as in-depth in some areas as we would have liked.
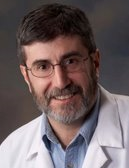
In addition to Inga, we asked a couple of industry experts to participate in the demo and provide their feedback. Our gurus included:
Dr. Gregg Alexander, who regularly writes the Intelligent Healthcare Integration columns for HIStalk Practice. Gregg is a self-described grunt-in-the-trenches pediatrician and geek.
John Smaling, an executive VP of strategic business development for Vitalize Consulting Solutions. He’s been in IT for almost 20 years, including stints at Paoli Memorial Hospital and Synexus Incorporated (which later merger with Daou Systems.) He’s also a hot commodity on the speakers’ circuit for events such as CHIME, HIMSS, and CIO Forums.
Note that the evaluation format we used was roughly based on the EMR Evaluation Tool originally designed by California’s Healthcare Foundation.
The lovely folks above are not really us, but we liked their use of scoring paddles. We actually used a 5-point scale for our ratings, with five representing the top score. Note that, in the interest of objectivity, we allowed athenahealth to look over the full review before it was posted and any points they felt were important.
If you would be interested in our reviewing your HIT product (preferably an EHR,) drop us a note.
Without further ado:
Overall functionality of product
Gregg: 5 – I felt the system flowed smoothly and enabled “chart jumping” – moving from section to section or page to page. I absolutely loved their “Prior Visit Tab.”
John: 5
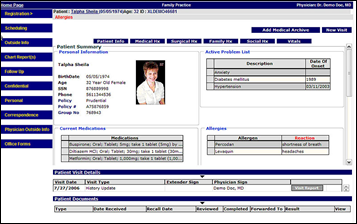
Inga: 5 – Seems pretty intuitive where to look to find different areas of the chart
Ease of documenting the visit and clinical decision-making process
Gregg: 5 – They have made great strides on their clinical side in regards to exam note or other document handling. The use of information “buckets” was intuitive and easily understood.
Inga: 5 – The system uses a lot of drop-down tabs that appear comprehensive and easy to use. A number of things are “auto-populated” into the chart, such a Surescripts data, lab results, and vital data (if interfaced with Welch-Allen).
John: 5
Ability to identify clinical issues by means of alerts and reminders
Gregg: 5 – As someone who has had a long penchant for office design and the interactions between design and workflow enhancement, I the ability to time each step in the care process is flat out hot. Also, athenahealth’s use of highlighting for various items and functions during the documentation process was simple, but effective. They helped provide focus being neither distractive nor overly intrusive. Their use of multicolored “flags” was also functionally useful.
Inga: 5 – Since athena is paid as a percentage of collections, they are obviously interested in incorporating tools that ensure patients return, and that the practice follows care protocols to ensure maximum reimbursement.
John: 5 – I particularly like the feature that times each step of the care process and earmarks opportunities for workflow improvement, based upon comparisons with the rest of athenahealth’s customers. This is a particularly effective capability and is a major contributor to their client’s attainment of a 1% increase in visits post-implementation.
Clinical support functionality
Gregg: 5
Inga: 5 – Includes use of First Databank. Since athena hosts the application, they can upload updates weekly.
John: 5 – Can have links to external knowledge sources such as Wolters/Kluher.
Prescription capabilities
Gregg: – 5 – Didn’t see (or don’t remember) if they can do weight-based dosing, something all pediatricians need with virtually every prescription.
Inga: 5
John: 5
Orders management, including interfaces with ancillary services
Gregg: 5 – Perhaps it is my small practice perspective, but as their percentage of collections fee for services is so reasonable, I found their handling of interfaces impressively 2009-ish, something I cannot say for a lot of systems.
Inga: 4.5 – I agree with both John and Gregg here. Is there a point that it is not cost-effective for athena to provide this? However, at this point it appears they are committed to providing and maintaining interfaces.
John: 4 – Interfaces are “built in” to the system, but the number and types of interfaces are factored into the monthly % of collections fee. As a consequence, they aren’t truly free. It is also unclear as to athena’s capacity to feed ambulatory transactions to a centralized repository to establish a longitudinal record inclusive of acute care episodes. Additionally, it would be interesting to understand how they would handle interfaces in the event that a major IDN purchased the product. In this case, they may have hundreds of pharmacies, 10’s of reference labs, and other 3rd party billing firms or other participants that would require an interface. Where is the limit and what could the cost truly reach?
Electronic communication capabilities with colleagues/patients
Gregg: Unknown.
Inga: Not covered
John: Unknown…this capability was not covered in the demo.
Athenahealth comments: athenaCommunicator provides not only patient portal functionality but a back office service that is fully integrated with athenaCollector and athenaClinicals to provide outbound calls to patients as well as electronic interactions. The portal provides for secure messaging between patients and providers and provides consumer friendly health information. It also connects with mainstream PHRs such as HealthVault.
Coding capabilities
Gregg: Not covered in the demo but with athenahealth’s tremendous reputation for the practice management side of things, I’d be inclined to think they have a targeting lock-on engaged for these issues,
Inga: Not specifically addressed, but athena doesn’t get paid unless the practice does; I would assume they have this covered pretty well. They do/will monitor whether or not physicians are doing all steps required to qualify for meaningful use.
John: Unknown…this capability was not covered in the demo.
Athenahealth comments: athenaClinicals is natively integrated with athenaCollector. Charge integration capabilities allow for translation of documented orders and procedures into CPT codes. Details of the visit translate into an appropriate E&M code for billing purposes via an integrated E&M calculator.
Compliance with rules and regulations on privacy, consent, etc.
Gregg: If I’m remembering clearly, we touched on HIPAA, but didn’t do the detail
Inga: Not covered.
John: Unknown. This was not covered in the demo.
Athenahealth comments: athenaNet, athenahealth’s centrally hosted national platform which houses all products is 100% HIPAA compliant and has been since 2003. We also have additional SAS70 Type 2 certification of our network. athenahealth is a covered HIPAA entity.
Aggregate individual data into longitudinal records for easy viewing and graphing
Gregg: 5 – Well done here
Inga: 5 – Graphs, etc. can be created on the fly. Pretty extensive capabilities.
John: 5 – Solid capabilities here inclusive of the ability to annotate in conjunction with the graphs
Ability to manage the individual patient’s chronic diseases and conditions
Gregg: 5 – I really appreciated some of the “look-back” abilities of the system.
Inga: 5 – Again, an area that athena is likely focused on as they help doctors with P4P programs, achieve meaningful use objectives, etc.
John: 5
Standardize disease management goals for subgroups of chronic disease sufferers within the practice
Gregg: Not covered, but I have suspicions they may have skills here cultured from their strong PM management tools.
Inga: Not discussed
John: Unknown. This capability was not covered in the demo
Athenahealth comments: We are set to launch by the end of 2009 a global P4P rules engine and service offering whereby the physician will be notified in real time of disease management information and data capture requirements. Athena specialists will enroll providers and will help monitor and submit data on behalf of physicians as part of this service. Unlike guidelines in traditional software systems, athena’s service team can monitor and inject rules into the workflow as part of this new service and which are available to all clients on the network at no additional charge.
Ability to query the system’s database to produce both individual and group reports on clinical issues — care, quality, outcomes, and associated costs
Gregg: Unknown.
Inga: Not covered
John: Unknown. This capability was not covered in the demo.
Athenahealth comments: Related to the P4P service offering, athenaClinicals includes population management reporting in addition to its existing suite of reports and reporting tools enabled by athenaCollector.
Ability to conduct research, registry, and clinical trial-related efforts
Gregg: Unknown.
Inga: Not covered
John: Unknown. This capability was not covered in the demo.
Athenahealth comments: Athena is in the process of becoming a PQRI registry for submission of data to CMS.
Incorporate information originating with the patient and, as a separate matter, with medical or patient devices
Gregg: I have a different take than John does, but I don’t know if it derives from this demo or another discussion I had shortly after this with another athenahealth rep during an unrelated interview. Their patient portal features are quite solid.
Inga: What is clear is that they have tools to input information not specifically generated from the chart note. Faxes are directed straight to athena and practices forward other data to athena for input.
John: Based upon the information covered in the demo, they are proficient at handling faxes and scannable content, they adhere to an HL7 standard, so feeding an industry leading portal/data aggregation product appears to be feasible. However, their inherent email capability wasn’t covered and I’m unclear as to the capability.
Usability and ease of inputting data using a variety of methods, e.g. keyboard/mouse, touchscreen, dictation, voice recognition, handwriting recognition
Gregg: 4 – I’m going to say 4 of these methods for sure, but I’m thinking they might hit all 5. They mentioned voice recognition, but I’m not sure about handwriting recognition.
Inga: 5 – They mentioned all these areas
John: Keyboard and mouse, but also I only recall them mentioning an ability to support light pen in addition to keyboard and mouse
Athenahealth comments: Yes we offer handwriting recognition, voice recognition, paper documentation, and transcription support for the provider.
Ability to customize capabilities to suit personal workflow preferences
Gregg: 5 – Demonstrator seemed comfortable with ability to customize, though taking the word of any EHR sales/demo guy can be a risky naiveté!
Inga: 5 – The indication was that pretty much every screen/template/process can be customized by user
John: 5 – Time did not allow for a deep dive into the customization capabilities of the product, but the demonstrator appeared very comfortable with the level of forms customization, screen flow, and other tailoring features of the app
Athenahealth comments: While athenaClinicals allows for customization we also leverage the knowledge and experience of our entire network to provide out of the box best practice configurations to optimize clinical workflow, speed of implementation and reduced cost of implementation and overall longterm ROI. We recently launched a five-stage patient encounter UX that integrates the patient visit workflow across Collector and Clinicals. This was launched to 100% of our Clinicals users overnight.
Screens are easy to interpret (menu categories, graphics, icons, and symbols)
Gregg: 5 – Though I initially thought the EMR appeared rather bland, their excellent use of white space, minimization of lines, rows, and columns, and their deft use of color for highlighting and focus won me over after a while. Flags, warnings, buckets, highlights, and chart-jumping were clear and easy to follow. Pop-ups signaling patient movement were nice. If we had a “4” ranking, I’d go with that as I still think some more color or perhaps some user customizable skins for individualization would be optimal.
Inga: 5– Personally I liked the fact the product isn’t overly “flashy.” Too much color and pop-ups can be confusing. The graphics and icons were intuitive.
John: 5
Integration with practice management systems and claims processing services
Gregg: Clearly 5
Inga: 5 single database for PM/EMR
John: 5
Access the EMR system remotely; ability to use a mobile devices
Gregg: Uncertain
Inga: Clearly can access the EMR remotely but we didn’t touch on its use via a mobile device
John: Unknown. This capability was not covered in the demo.
Athenahealth comments: athenaNet is the only centrally hosted web native platform, meaning that it was specifically designed to be accessed anywhere at any time over the internet. All of our services, including athenaClinicals, are delivered via this web based platform.
Process, exchange, and store graphics and images
Gregg: – 3 – I’m going to grant a 3 here as our discussions on fax/chart/paper document scanning leads me to feel comfortable that imaging issues are probably well-considered, but I cannot verify PACS/RIS nor DICOM from our demo.
Inga: – 3 ditto Gregg’s impressions
John: Unknown. This capability was not covered in the demo.
Athenahealth comments: athenaClinicals will easily interface to a RIS/PACS system so that images can be launched in those systems in the context of the clinical visit or image review process.
Overall Impressions on functionally, intuitiveness, graphics, overall flow
Gregg: 5 – From the grunt in the field level, athenahealth should be near the top of the EHR consideration list. The abilities facilitated from the practice management side are significant. The work transferable to athenahealth from the practice management side should allow office staff a much greater focus upon patient care issues. Having more folks in the office more directed upon real care issues and not business operations should be attractive to anyone who still wants to provide healthcare, not just run a business. athenaclinicals are developed enough and intuitive enough to rate a 5. (Well, technically, it’d be a rounded-up 5, but a legitimate top-ranked EHR on my scale.)
Inga: 5 – I had looked at the product a year or more ago and found there to be a number of gaps at that time (e.g., templates were not as complete.) However, the system has matured. athena’s approach may not be for everyone, but it’s fantastic for a group that does not want to have to worry about the IT “stuff,” like loading regular updates. Also, it would be great for the practice that wants to minimize in-house staff for mundane tasks like document imaging. Also for physicians who don’t want to worry about learning about all the meaningful use rules, but prefer to have someone tell him/her what is required and leave it at that.
John: 4 – Not to be difficult, but the demo was too brief to provide a thorough rating. My sense is that athena has made great strides with their product, but it may be more attractive to smaller practices or even larger groups who have no desire to invest in an internal IT capability. IDN’s may find the SaaS thrust of the product to provide a degree of constriction that they would find unattractive. Again, these are extremely high level observations and I wouldn’t stake my professional reputation on them; not that I have one to begin with!
I would use this in my practice and/or recommend to others
Gregg: 5 – I would definitely rank athenahealth near the top of my “Overall Smokin’ EHRs” list.
Inga: 5 – John makes a good point that this model may not be for everyone. But from feature/function/ease of use standpoint, it appears very solid.
John: 4 – I would qualify this by saying that it may be a good fit for many standalone practices, but IDN owned or strongly affiliated practices may find this model a bit wanting.
















The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…