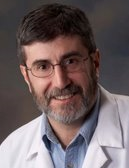
HIStalk Practice Interviews Andrew Baumel, MD
Andrew Baumel, MD is a pediatrician with Framingham Pediatrics of Framingham, MA.
Give me some background on the practice.
 We’re Framingham Pediatrics and we’re at FraminghamPediatrics.com, if you want to check out our Web site. We are a six-person pediatric practice. We have six MDs, no NPs or PAs. We have about 10,000 patients in the practice. We’re in suburban Boston just about 20 miles out of Boston. We treat a very mixed population, socioeconomically and demographically.
We’re Framingham Pediatrics and we’re at FraminghamPediatrics.com, if you want to check out our Web site. We are a six-person pediatric practice. We have six MDs, no NPs or PAs. We have about 10,000 patients in the practice. We’re in suburban Boston just about 20 miles out of Boston. We treat a very mixed population, socioeconomically and demographically.
We’re affiliated with MetroWest Medical Center in Framingham. We’re also a member of the PPOC, which is the Pediatric Physician’s Organization at Children’s Hospital. It’s an over 300 doc group in the surrounding Boston. We recently signed a contract to eCW to put eCW in all the practices in the group.
We had already been with eCW since 2005, so we’re kind of ahead of everyone else and everyone else is being implemented over the next 12 months. But we started with the technology back in 2001 when we were part of an e-prescription pilot from Blue Cross/Blue Shield, and then we moved in 2005 to EMR.
In 2005 I was really looking for just a replacement for our practice management system because ours was going defunct. It was called PSI. It was out of Rhode Island and their company was bought by Pulse and Pulse just assumed well, we’ll just jump to their EMR, but it was not a good product. So I was looking for a new practice management system, looking at a lot of ASP models, and I found a couple EMRs that were actually less expensive than just the fee on the loan, and one of them was eCW. And I actually met the eCW people at Pri-Med’s conference in Boston that year and liked it and I said, “Gee, if I can spend less money and get the whole thing, why don’t I do that?” It’s great.
So we went with it. In February 2005, we went live and I’ve been to four annual user group meetings with eClinicalWorks. Those conferences were amazing. Girish and everyone said, “Just rip us apart. Tear it down and build it back up. What do you want to see in the program? Where can we have less clicks? What do you want?” And the program I was using in 2005 is totally different than the program I was using now. It just keeps evolving and every iteration gets better and better.
A lot of the really cool features I kind of had a hand in, along with all the other doctors at these conferences, such as the patient dashboard. They’ve come up with some really cool things lately. I’ve been really excited about the registry in the patient portal. We have been using registry a lot and it’s really amazing because we really concentrated in the beginning on doing a good job on making the problem list readable and having the problem list be relevant. By doing that, you can run really robust registry reports. We’ve had the patient portal going for the past three months and we’re up to 2,900 patients out of 10,000, which is a nice job, I think.
We’ve been able to leverage that for our notification of the flu shot as it’s coming in, both the seasonal flu shot and the swine flu shot. We’ve been running reports based on children’s special health care needs using our registry searches to send e-blast messages through the portal. For example, last week we got in a batch of H1N1 vaccine and we decided to give it to our sickest patients first, then to asthmatics. With a couple clicks of the registry we found who has asthma. I think it was 500 patients, of which 240 were Web-enabled. We sent out a quick message saying, “The swine flu vaccine is in we’re running a clinic tomorrow afternoon, make an appointment.” Within 40 minutes, we had 55 appointments set.
The future for the portal is amazing because I can send out directed messages to certain subsets of my population immediately and have them respond. For example, there’s one town in our area that doesn’t have fluoride in the water — Ashland, Massachusetts. In Ashland, at the six-month visit, we put all our patients on fluoride. We can send out a message to all our four-month-old patients, and four-month and six-month old patients who haven’t been in for their visit. We send them an e-message that also explains how the fluoride is administered so we don’t have to do that during the visit.
Or, when albuterol went off the market; it went from generic to brand name. We had to switch all our patients from albuterol to ProAir because it doesn’t have any hydrofluorocarbons killing the ozone layer. When patients didn’t get a refill on their albuterol, they would call and ask why. If we had had the portal set up six months ago, we could literally catch every single patient on albuterol with a current prescription and send them an e-blast saying your next script will be for ProAir and this is why. We would have saved so many phone calls.
And, let’s say a vaccine lot or a drug is recalled. I could search my registry for subsets of patients then I can send them out an e-message. It’s just going to be amazing. My partners always ask me, ‘When is this EMR going to make healthcare better?’ Well, this is the answer — being able to communicate in this other way.
I was home yesterday. I got five Web messages and I responded to them from home. It saves phone calls. It was asynchronous communication. And our Web portal saves that conversation as a visit in eCW. On the mom’s end, it saves our conversation in her portal page to always go back and refer to it.
And when I get that Web message, it’s within the patient’s chart, as opposed to an e-mail that the secretary prints out, gives to you, and then you look up the patient’s chart. That’s the thing I’m most excited about recently.
Has the passage of the ARRA changed your focus at all in terms of technology adoption?
Not at all. Most of my colleagues are, like myself, not eligible because we don’t have any elderly patients, so we don’t have Medicare. But I’m the largest Medicaid provider around, personally, and I have 20% Medicaid, which may qualify me for ARRA, but the whole practice is about 12% Medicaid. We’re in an area with plenty of poor patients and we see them, but pediatricians won’t qualify under those restrictions. Plus it’s short money. It’s $44,000 over four years. That’s not a lot of money.
What about pay-for-performance programs?
Well, we’re moving beyond that, actually. We have one of the newest, latest flavor of contracts in the country. PPOC made a deal with Blue Cross/Blue Shield of Massachusetts. They gave us a $10 million grant to do a product for the Patient-Centered Medical Home. Our practice is a leader in the area because we were first with the EMR. We have now implemented the Patient-Centered Medical Home in our practice, mainly leveraging our EMR to do it. We’ve identified all patients with special healthcare needs; we had identified them in the EMR. We’re getting care coordinators in the offices and are now doing initiatives on attention deficit, Down syndrome, and asthma care.
We’re all following evidence-based guidelines, making sure we follow-up. We’re doing referral tracking and identifying critical referrals through the EMR, then checking to see if they were done and if we’ve gotten a note back. We’re following up on how quickly we get back to patients when we’re taking a call at night or when they call the office. We’re doing the whole Medical Home project and we’ve been incentivized by Blue Cross through a contract with the PPOC to do this.
We have these 10 core elements that we’ve had to document and identify and do and measure. We’re able to really leverage the registry and four years of data in our EMR to really become a Patient-Centered Medical Home for our patients.
Why do you think EMR adoption in general still remains low?
I think that it’s pretty hard to put down the pen and paper. Doctors have always done it a certain way and they don’t want to change. Changing’s hard. It takes a few years to reap the dividends of EMR. Plus, a lot of specialties aren’t really geared towards EMR. Whereas, pediatrics is perfect for EMR because every two-month visit pretty much follows the same script. Every one-month visit has the same shots. So many visits are well-scripted and you do and say the same thing over and over and over again. I say the same thing over and over, but I can do one click on a template and it’s all there written for me.
With eCW, everyone can have their own template. Every single note in the system is a template, essentially. I can pull up any note and copy it, so I don’t have the same six-month-old template as my partners do. Everyone has our own so it’s in our own words. So the EMR’s working for me, I’m not working for the EMR.
The problem is that to get there, you have to be interested in doing it. You have to invest a lot of time and effort. You’re not willing to put in that time and effort if you’re a solo-practitioner and there are only two people in the office, or you just don’t have that curiosity to do it. I personally find it fun and interesting and I think it’s efficient. It’s really improved my ability to take care of my patients and now we’re just going to take it to the next level. But most doctors don’t want to make that change; the investment. They’re just scared, and it’s so easy to write it on paper.
I was very involved the e-prescribing pilot with Blue Cross/Blue Shield and 200 doctors got handhelds. And out of 200 doctors, only nine of us used it more than 50% of the time to write scripts. Of those people, six of them were in my office and 99% of our scripts were written on e-prescribing machines — and why? Well, the handhelds didn’t come pre-loaded with our favorites list, so before I gave it to any of my doctors, I loaded all our favorites. It made it easier to use than to write it on paper. Refills were a snap. eCW’s not a turnkey product, but I set up the e-prescribing and I set up eCW to run just perfectly before it got in their hands so they wouldn’t get frustrated. A lot of docs aren’t going to have that because their EMRs are not turnkey solutions.
Then the other very secret thing is that most EMRs stink. When people start using other EMRs and say, “This EMR is slowing me down on patient care; it’s taking me forever to write a note.” Whereas, when I walk out of the room, frequently, my note’s finished because I run the tablet and I’m just writing in the office, using a pen or typing. I get out of the room, maybe I’ll add my treatment thoughts and finish the billing, but my note’s essentially almost done when I leave the room. But some EMRs are so bad and I can’t believe some of these things are still being sold. So in terms of why people aren’t adopting it, well, their colleagues say the EMRs stink.
If people tell me that eClinicalWorks is bad, I say, “Well did you do this? Did you do that? Did you write a template? Did you customize this?” They say, “No, we didn’t, we just started using it.” Well of course it’s not going to be good if you don’t customize it. It comes as a plain, generic thing and then you just have to make a few pick lists and templates, which are really easy to do. They just never take the time to do it. It’s like saying my car won’t start. Well, did you put gas in it? Well, no, we just bought it and tried to start it but there isn’t gas and to won’t run. Well of course not, you have to buy gas. They don’t do the simple, simple things that you need to do to get the EMR running efficiently. So I think it’s going to take a long time before EMR is fully adopted.
And what’s interesting now is we’re moving from the early adoptive phase to the phase where now its large organizations are buying EMRs and forcing their individual doctor practices to use it. That’s going to be a really, really tough phase for the industry because these people don’t want to use it. No one’s enthusiastic. You poison the whole office because if you grumble about it, the nurse’s aren’t going to use it. They’re still going to write you little telephone notes on paper and give it to you. They’re not going to use the telephone encounter. If the doctor’s aren’t enthusiastic about it, it just ruins it for everybody and no one’s going to use it.
So I think it’s going to take a long time. Massachusetts is the most advanced state for EMR in the country at this point, but it’s going to take awhile before everyone adopts it fully. But I still can’t believe that people are buying these bad, bad systems out there.


















The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…