Re: Walmart Health: Just had a great dental visit this morning, which was preceded by helpful reminders from Epic, and…
From the Consultant’s Corner 8/7/19
Patient Access Centralization – Far More Complicated Than Anticipated
By Nancy Gagliano, MD

Nancy Gagliano, MD is CMO at Culbert Healthcare Solutions in Woburn, MA.
Over the last decade, healthcare organizations have implemented centralized access centers with the promise of a panacea to improve patient satisfaction, access, volume, revenue, and all that ails ambulatory operations. Numerous articles have espoused the value of this approach. Unfortunately, organizations are struggling with numerous challenges, having underestimated the complexity involved in running a successful patient access center.
The wide variety of challenges are not easily covered in one article. This article will summarize and highlight common opportunities. Over the next few months, I’ll dive deeper into these challenges, highlighting considerations and recommended solutions. Topics will include:
- Scheduling templates and governance.
- Technology and telephony.
- Staffing and service level agreements.
- Establishing a patient access center approach.
- Self-service – where the future lies.
“Centralized Patient Access” does not have one clear definition. In some organizations, it defines the approach to registration and insurance verification. In other organizations, it includes scheduling and referral management. In some, it also includes pre-authorizations and nurse triage. Without a clear short- and long-term vision, organizations struggle with whether this is a finance or an operations unit. When the initial foundation and governance is not clear or aligned, it leads to broader challenges as a centralized approach is expanded. In some organizations, we have seen two central access groups – one for financial-related activities and the other for patient clinical activities, creating unclear accountability. Other organizations have one center but are challenged because of matrixed responsibilities and structure.
Scheduling: A common scenario includes scheduling staff centralized into pods of expertise responsible for registering and scheduling patients. Patients, in theory, will be evenly distributed to all available providers, filling any open slots, and providing access quickly to patients, resulting in increased patient satisfaction and overall volume. While organizations are aware this works best when schedule templates are simplified with clearly documented protocols, the hard work of obtaining provider buy-in and changing their schedule templates is often not completed due to provider resistance. Without simplified schedules, the patient access center often makes errors as well as ends up with unused slots in schedules. Without easy access to talk to providers, schedulers cannot fill unused slots for “different” patient types. It is often best for central access centers to start with more general specialties, such as primary care, and then add complexity associated with specialties as the foundation for success is established.
Governance: An opportunity often underappreciated is the need for a governance model that has accountability for both the performance of the central access unit and dependent clinical operations components. For a centralized unit to be successful, a collaborative dyad between the practices and the central unit is required. An organizational approach to scheduling templates, visit times, provider availability, and bump rules needs to be defined and managed. Practices, in turn, need to be assured of appropriate staffing, training, and performance of the centralized unit. Working together through joint governance creates the collaborative approach necessary for the foundation of success.
Technology and Telephony: There are numerous third-party vendors available to support effective call center operations. Many organizations leverage telephony and provider matching systems already in place. However, for efficiency and quality, additional systems can be extremely helpful. I have seen organizations have too many systems, too few systems, poorly leveraged systems, as well as a lack of internal expertise to maximize the use of technology.
Staffing: Appropriate staffing for call centers is quite complex. Turnover is often as high as 30% – higher than ambulatory practices. Replacement staff tend to lack training, experience, or exposure to the clinical setting, and are therefore less efficient and prone to errors. Given high turnover, most centralized call centers are short staffed, particularly on Mondays and Tuesdays, in addition to most mornings, which see peak call volumes. Appropriate staffing is also dependent on which specialties are included in the access center. The more specialized the departments are, the more complex access support is, requiring a higher level of staff skill.
Us/Them Mentality: When practices have their staffing cut to support a central unit, it commonly sets up tension between the two. Practices may want all calls to be handled centrally and are often slow to respond to calls from the call center in need of support and clarification. Practices may undermine the central unit by providing patients with a “back number” to the practices. Or practices will avoid scheduling any patients, such as follow-up when leaving their visit, and refer all scheduling events to the call center. In turn, call centers voice frustration on calls they receive that may not technically be their responsibility, such as medication refill requests or complaints that the practice hasn’t returned the patient’s calls. The antagonism is typically not anticipated or realized until the center is underperforming and improving relationships is difficult.
Patient Satisfaction: While patient satisfaction and consumerism are often a core rationale for centralized patient access centers, underperforming central access may worsen patient satisfaction. Poor response times, handle times, errors, and lack of expertise may lead to dissatisfied patients who find back channels to the practices to get their problems solved. Subsequently, providers and practice leadership, vent their frustrations to organizational leadership.
Referring Providers: An effective patient access center is designed to efficiently handle referrals to minimize leakage and reduce the work by outside practices to schedule their patients. Unfortunately, many call systems are still working through faxed referrals, resulting in only about half of the requests ending in actual patient visits. To complicate matters, most organizations do not have an efficient tracking process to inform referring providers of complete or incomplete referrals.
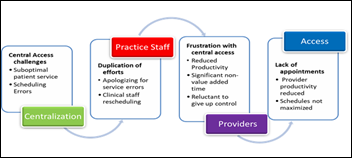
Cascade of Challenges: The result of an ineffective patient access approach is a cascade of challenges. The central patient access center is challenged in meeting call demand and is fraught with scheduling errors. The practice staff spend time cleaning up schedules, rebooking patients, and dealing with frustrated patients. Because practice administrative staff numbers have been transferred to the central unit, the time spent in “clean-up” precludes practice staff from supporting in-office patient flow and other patient needs. Subsequently, providers are less efficient, frustrated with the central unit, and often request being removed from the central until. The overall result is frustrated patients, providers, practice staff, and access staff without significantly increasing access, productivity, or reducing costs.
If operating a superb patient access center isn’t challenging enough, most organizations initially set up their centers for phone-based interactions with patients. Now access centers are transitioning to multi-channel communications, because patients want the ability to communicate by phone, text, email, and chat. The next goal for organizations is to support patient and referring provider self-service. However, without setting the above foundations, self-service will only be a vision for the future rather than a near-term reality.
In summary, operationalizing a patient access center is extremely challenging and many organizations are looking for ways to improve performance, patient satisfaction, and provider engagement. While there are no quick fixes, organizations should assess their vision, governance, provider scheduling approach, technology, and staffing. Stay tuned for deeper dives into these topics.
Contacts
More news: HIStalk.
Get HIStalk Practice updates.
Contact us online.
Become a sponsor.

