News 7/7/11
National Coordinator Farzad Mostashari MD concurs with the HIT Policy Committee’s recommendation to push back the start of Stage 2 Meaningful Use by one year. Reason: the rule includes a January 1, 2013 start date for Stage 2, but the Stage 2 requirements won’t be finalized for another year, leaving EPs, hospitals, and vendors insufficient time to prepare.
Symantec and Allscripts partner to offer an online privacy and risk assessment tool that allows practices to identify potential gaps for complying with HIPAA rules and HITECH. The application can be deployed with any EHR and not just Allscripts products.
No surprise here: a study of HIT implementations in small practices concludes that not early all adopters believe the investment was worth the time and money. The biggest problems cited by providers include technical difficulties, lack of training offered, lost productivity, and the inability to get systems to talk to other EHRs.
Primaris, Missouri’s Medicare QIO, collaborates with e-MDs to provide free assistance to e-MD users interested in earning PQRS incentives for 2011 and 2012.
Premier Purchasing Partners awards SuccessEHS a 36-month contract to offer its group purchasing members special pricing on its EHR, PM, and billing services.
OptumInsight partners with RemitDATA to offer the Web-based Remit Advice Professional service, which gives practices access to analytics of remittance notices from health plans, along with coding and reference tools. OptumInsight (formerly Ingenix) is part of United Healthcare’s Optum business unit, which just named Larry C. Renfro its new CEO. Outgoing CEO G. MIke Mikan is leaving to head up a private equity fund.
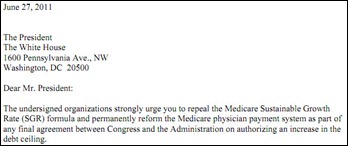
CMS issues its proposed fiscal 2012 Medicare payment rule, which includes a 29.5% pay cut for physicians. The drop in reimbursement reflects the current SGR formula, which CMS administrator Donald Berwick, MD says must be fixed to avoid “serious consequences.” The proposed rule also expands CMS’s misvalued code initiative to update codes that over- or under-paying providers. If CMS’s proposed changes to telehealth services are approved, telehealth access and the types of eligible services could be expanded: the proposed rule places more emphasis on telehealth’s clinical benefits, rather than requiring a telehealth visit to provide all the same exam elements as an in-person visit.
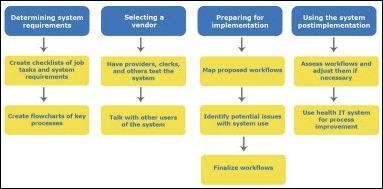
AHRQ and the University of Wisconsin-Madison’s Center for Quality and Productivity Improvement develop a toolkit to help practices in workflow analysis and redesign before, during, and after HIT implementation. There seem to be a good number of toolkit options available, ranging from benchmarking, checklists, and flowcharts, to interviewing, risk assessments, and usability evaluations.
EHR and PM company ACOM Health buys billing service provider Contract Medical Billing. The service will be rebranded as ACOM Medical Billing.
Aria Health (PA) selects Allscripts Community Record to enable data sharing between the Allscripts Ambulatory EHR used by its employed physicians and Allscripts Sunrise used by its hospitals. The community record technology is powered by dbMotion and will also tie in other regional providers who use non-Allscripts EHRs.















Re: Walmart Health: Just had a great dental visit this morning, which was preceded by helpful reminders from Epic, and…