News 6/9/11
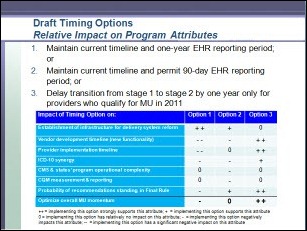
The HIT Policy Committee advises ONC to push back the Stage 2 deadline for Meaningful Use to 2014 for providers who qualified for Stage 1 this year. The committee believes the original timeframe does not give providers or vendors adequate time to prepare for Stage 2, especially since the final Stage 2 rules will not be released until June 2, 2012. The proposed change would allow providers to collect Stage 1 and 2 incentive payments for two years without penalizing early Stage 1 adopters with a tight Stage 2 deadline.
Shareable Ink partners with Waiting Room Solutions to combine its digital pen technology with the EHR from Waiting Room Solutions.
Spring Hill Primary Care (WV) contracts with Sage Healthcare Division for the Intergy Meaningful Use Edition.
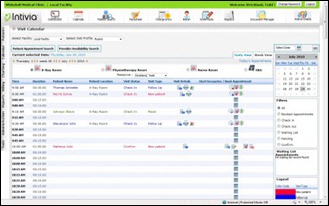
Initivia will extend special pricing for its InSync EMR/PM product to members of Premier Purchasing Partners, a group purchasing organization.
The Louisiana Care Quality Forum REC designates Greenway’s PrimeSUITE EHR as a supported EHR product.
CRISP, the REC for Maryland, meets its subscription goal with the enrollment of 1,000 primary care physicians.
CMS adds a few questions to its FAQ page on the EHR incentive program. Here are a couple of the better ones:
What information must an EP provide in order to meet the measure of the meaningful use objective for "provide patients with an electronic copy of their health information?”
The minimum required information includes a problem list, diagnostic test results, medication list, and medication allergy list. CMS also notes the four elements must be provided to patients within three business days of their request.
For the Medicare and Medicaid EHR Incentive Programs, when a patient is only seen by a member of the EP’s clinical staff during the EHR reporting period and not by the EP themselves, do those patients count in the EP’s denominator?
The EP can include or not include those patients in their denominator at their discretion as long as the decision applies universally to all patients for the entire EHR reporting period and the EP is consistent across meaningful use measures. In cases where a member of the EP’s clinical staff is eligible for the Medicaid EHR incentive in their own right (NPs and certain PAs), patients seen by NPs or PAs under the EP’s supervision can be counted by both the NP or PA and the supervising EP as long as the policy is consistent for the entire EHR reporting period.




















Re: Walmart Health: Just had a great dental visit this morning, which was preceded by helpful reminders from Epic, and…