Farzad Mostashari MD is founder and CEO of Aledade.

What has the last year been like for Aledade? You mentioned in an interview with Mr. H last year that it will take the “right tools, right tech, right booths on the ground, with the right team, with the right primary care providers” to really make progress in achieving the triple aim. How have those factors come together for your team and clients?
It’s been super fun for me. It’s so totally unlike the federal service, but there’s also a similarity as well. It does feel like we are embarking on something that really matters and that has the potential to impact a whole lot of people. It does feel like I’ve been training for this my whole career, pulling on the skills around analytics, technology, and change management in small practices to start an operation that’s small today, with the ability to be successful when it’s really at scale. We’re keeping our eye on the prize and feet on the ground. We always talked about that at ONC. That’s really what Aledade, if you recall, is all about, keeping your eye on the prize, on the North Star.
Process-wise, it’s been amazing to grow the team. We’re now 25 people, and we’re hiring one or two people a month. We are looking for EHR implementation specialists right now – people who are ninjas with some of the larger ambulatory EHR systems – to really do that turbo charging, that optimizing, that me and our doctors certainly feel is lacking. They have the systems but they haven’t been optimized, and so that’s something we’re engaged in actively with our practices.
We’re growing as the flurry of recent press releases has attested. We started off in four states – New York, Maryland, Delaware, and Arkansas – last year. This year, there’s been a great reception to this idea of independent primary care providers being able to take on these new alternative payment models for which, frankly, they are in a great position to succeed and thrive at with help. We’re now in Kansas. We’re in West Virginia. We’re in Louisiana. We’re in Tennessee, and there’s another state soon to be announced.
Has your business model changed over the last year?
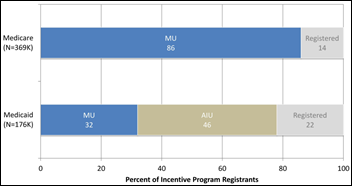
No, it’s still the same basic model. This whole alternative payment model thing says you get paid for outcomes, and our business model is still predicated on showing outcomes. There’s a pretty small membership fee to make sure the docs are committed, but our interests are lined 100 percent with the payers, and with the providers and the patients. Participation in Meaningful Use is still a requirement to work with us, and most of our partner doctors are working on stepping up to stage two.
How many practices and patients does Aledade now serve?
We currently operate three ACOs across four states (DE, MD, AR, NY), covering nearly 30,000 Medicare beneficiaries. Additionally, we are currently undertaking physician recruitment in several other states, including Tennessee, West Virginia, Louisiana, and Kansas.
How are you handling distributing payments to the individual providers Aledade works with?
As you know, in the Medicare Shared Savings Program, ACOs receive 50 percent of the savings they achieve against Medicare predictions of cost of care. Of that amount, 60 percent is distributed to our individual practices, with 40 percent reinvested in further improvements to the ACO.
Your time at Brookings helped you to better understand what makes an ACO work and what doesn’t. Have those findings generally held up now that you’re seeing ACOs from a boots-on-the-ground perspective?Absolutely – and interesting that you use the phrase "boots on the ground." While at Brookings, we identified four key competencies for running a successful physician-led ACO:
- Identifying and managing high-risk patients.
- Developing high-value referral networks.
- Using event notifications for hospital admissions, transfers, discharges, and other similar events.
- Engaging patients.
A little less than a year into running Aledade, we believe those conclusions even more strongly. We’ve learned a lot from our practices – as well as our regional partners – and it is truly these capabilities, coupled with our data and analytic expertise, as well as the work of our regional partners, that have helped our ACOs succeed thus far.
The foundation of all of our ACO success though, has really been the identification and engagement of top physician leaders everywhere we’re running ACOs. We’ve been fortunate to partner with docs who are leaders in their communities, are well-versed in EHRs, and, most importantly, share our vision and values for what ACOs can accomplish.
How have Next Generation ACOs impacted your business? Are your practices interested in it?
I really appreciated the Next Generation ACO proposal. Maybe not this year, but next year I think some of our ACOs will be ready to take on that challenge, especially if there are some tweaks made to that model. That’s what, to me, is the most significant part of this type of ACO. It’s further evidence that CMS is committed to figuring this out. This is not a one-shot experiment. There are a whole series of efforts to tweak and modify and work on and adapt and evolve the fundamental ACO model until they find one that really will serve patients, providers, and payers. That to me is the bottom line, not a take it or leave it kind of situation. CMS really wants to work with the providers to make a model that works.
You’ve mentioned that EHR optimization takes up a good bit of Aledade’s time. What type of optimization challenges are you running into the most?
We really want to have the EHRs at the top of their license, and so we need to help the providers be absolutely certain that their systems are not only capable of meeting MU certification requirements in the lab but also in the field. It’s been a little unsettling to see how many certified EHRs providers upgraded to that can’t perform in the real clinical setting. Take portability requirements, for example. They got tested to them in the lab and they could certainly do it in the lab, but they’re not really able to perform that certification function in the field.
This has been something that I was super happy to see ONC take on squarely in the notice of proposed rulemaking. This was also, frankly, what the congress touched on when saying ONC should decertify systems that are, for example, blocking information. It all comes down to not necessarily more requirements to certification, but making sure that the requirements that are there meet the intent and satisfy the customers, and to have a mechanism for customer complaints if they’re not getting what they thought they were buying. It would be beneficial for the certification bodies to do a small sample of practices and actually get in the field and say, "We’ve tested it in the lab, but we’re going to go and test five or 10 practices in the field and make sure the systems are capable of doing what they’re supposed to be doing."
Have you had to assist any in selecting a new EHR?
There are, unfortunately, a number of our practices, and I don’t think they’re unique in this, who are unhappy with their systems, particularly if they’re a little bit older technology. The optimization, the interfacing … it’s just getting so painful for them, so they ask me, "Look, you’re the formal national coordinator for health IT, tell me what should I switch to?" One of the things I’m actually going to be doing at HIMSS, and this is going to be quite interesting for me, is walking around in the mind-frame of a customer, someone who’s looking to buy an EHR that really meets the criteria for practice happiness. A system that is able to achieve MU requirements in a thoughtful and workflow-optimized way, and has the willingness and interest in working with third-party population health applications. Those are the three criteria that I’m going to be looking for so that we can make educated recommendations to our practices who do want to switch systems.
Were there any rumblings from physicians about the 10-year interoperability roadmap? How does that play into your plans for them and how might that be shifting what they had originally intended to try and achieve with their EHRs?
For a lot of the small practice primary care docs, the interoperability that really matters to them is functional interoperability. It’s having their lab results be in their system electronically. It’s having a discharge summary or a referral be sent electronically. It’s being able to electronically report their immunizations to the state immunization registry. Their expectations are not very fancy.
There are two things that have come up that I think the interoperability roadmap intersects with very directly. One of them is that it is incredibly helpful in running an ACO to have technician discharge transfer notifications. If there is one HIE function from a public or private HIE that I would prioritize for population health, it’s just that simple HL7 ADT-fed notification of admissions, discharge, and then transfers, which is considered pretty bare-bones for an HIE. That’s where there’s so much value today. I think more HIEs should first focus on delivering what people actually need today for population health.
The second interoperability challenge that is really top of mind for these practices is, in many cases, that they have spent years inputting data into the systems that they have paid for, and now, to get their own data out of those systems, they’re having to pay the vendor $5,000 to $10,000 for an interface. We’re covering that cost, but it’s outrageous. What we really want is basically the CCDA that they, for certification purposes, are supposed to be producing anyway. Those are two things that I would highlight as being key, functionally, for ACO participants.
Given that you see so many EHRs and different types of vendors, have you seen them paying more attention to population health management?
It’s the big buzz word, right? That and patient engagement, and soon to come, precision medicine. Everyone talks about it and I feel like saying, “Look, we gave you a roadmap for what population health requirements are. It’s called Meaningful Use. If you had really embraced the intent behind Meaningful Use, you would have not only not frustrated your customers with a compliant approach, but you also would have had a leg up in this new value-based world. It is exactly those things. It’s decision support. It’s tied to quality measurement. It’s quality measurement at the time of care. It’s registry functions. It’s having and sharing data needed for identifying high-risk patients and managing their conditions. It’s safety around medications. It’s engaging patients to be partners in their own care. It’s giving them care plans. It’s all there. Now they are, in many cases, touting their population health bona-fides as if they had discovered it for the first time.
In working with different practices in different states, have you seen any using their EHRs or other types of health are IT creatively, in a way that you thought might work for a different provider in a different part of the country?
Yeah, absolutely. Holly Dahlman, MD is at one of our practices, Greenspring Internal Medicine near Baltimore, and she is a nationally recognized Million Hearts champion. She’s doing amazing work with hypertension control. Her use of the EHR is fairly sophisticated. She uses registry functions to identify unrecognized, under-diagnosed, or under-treated patients so that she can then work to engage with them on their heart health. She’ll then initiate home monitoring and reporting of blood pressures from home monitors into her system. It’s great to see one of our practices being one of the stars in that initiative. We’re rolling that out to our other practices.
How many RECs do you interact with? How have you seen their role evolving (or drying up) as EHR adoption plateaus?
Right now, we have partnerships with eight RECs – in New York, Delaware, West Virginia, Tennessee, Kansas, Louisiana, Florida, and Arkansas. As EHR adoption has plateaued over the last year or so, the role of the RECs has evolved, and possibly become more important. Even as EHR market penetration has increased, we’re seeing doctors and their office staff still struggling with operability of some of these systems – not just functionality with other systems, but functionality on their own systems, accessing their own patient data. Some of this has to do with business practices of some EHR vendors, but regardless, the RECs have been there, on the ground with these practices, working to help them get the highest level of functionality out of their system. They are an invaluable piece of on-the-ground support for independent physician practices, and that’s why we’ve chosen to partner with so many of them.
Do you have any final thoughts?
Health IT and delivery reform are twins. You can’t get the full value of each one independently without the other. You can’t do these new payment models without pretty sophisticated use of information technology, but this is a point that is often lost. A lot of these population health-oriented, prevention-oriented, care coordination-oriented technologies don’t make sense in a fee-for-service world, but they make perfect sense in a world where people are paid for outcomes. For the HIStalk listeners, their work in making health IT that works has never been more needed and more significant, and this is going to go not only to the professional and healthcare desires to take the best care possible of patients. It’s actually going to determine the financial and business viability of their organizations; so kudos, keep up the hard work. I’m cheering on both populations.
Contacts
Jennifer, Mr. H, Lorre, Dr. Jayne, Dr. Gregg, Lt. Dan
More news: HIStalk, HIStalk Connect.
Get HIStalk Practice updates.
Contact us online.
Become a sponsor.




























Re: Walmart Health: Just had a great dental visit this morning, which was preceded by helpful reminders from Epic, and…