Practice Wise 3/30/12
EMR is the Great Magnifier
Paper processes do an amazing job of hiding practice dysfunction. Many doctors start their independent practices because they want to practice medicine their way. They hire staff to perform the front desk, bookkeeping, and nursing tasks. They provide good patient care. The insurance claims go out, payments come in, bills get paid, and they take home a decent salary, so things seem to work fine for them.
But it is common that there is nobody in the practice who has a strong grasp on process development. Each staff member or team builds their own processes and guards their own turf. The practice runs on the tribal knowledge of staff.
When we assist clinics through their EMR implementation, we first do a process map with to approximate how their paper workflows will translate to the EMR. The staff tells us what their processes are when we are on site to observe their paper workflows. What we ultimately discover is that their actual processes are often so different that we question whether these workflow mapping activities are even fruitful.
When we are mapping workflows and doing on-site training, we tune into the staff dynamics. There is a common disconnect in many practices between the reception staff and the billing office. The receptionists think the billers are nags who don’t trust them to do their jobs and who hoard information from them. The billers think that the receptionists are not capable of getting the appropriate insurance information from the patients to generate clean claims, so they don’t let them complete patient registrations. They often hinder the claims process by hoarding rather than sharing information that could empower the receptionists to be the front line of the billing office.
Then there is the power tussle between the nurses and the schedulers. Schedulers don’t want the nurses messing up their schedules so they ask us not to give them certain appointment booking privileges. Nurses want to control the same-day appointments and don’t want the front desk to have that power over their schedules.
We see these dynamics over and over again and try to address them all the way through the implementation process. Although these dynamics existed when practices went live on various practice management software products in the past, the providers were usually unaware of the power struggles amongst their staff because the PM software rarely engaged them. Now that the providers are engaged in the EMR implementation, these same dysfunctional behaviors are affecting them.
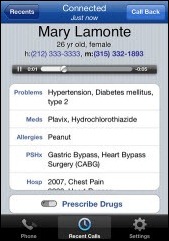
Doctors have their own dysfunctional behaviors that become glaringly obvious when they go live on EMR. When using paper charts, it’s likely that nobody is verifying how they chart, when they chart, or even if they are fully charting a visit. They can complete a fee ticket/superbill and turn it in to billing — a claim gets processed and the paper chart gets filed.
A good EMR will require them to chart appropriate elements according to coding guidelines. I’m amazed when the doctors get mad at us or the EMR product for “making” them chart appropriately. They get mad about how many clicks it takes them to complete a note. Although they are charting more complete notes that protect them and their patients, they want to do it all in three clicks or less, yet make it comprehensive enough to generate a robust letter to the referring physicians and reap the maximum reimbursement.
They often remove items from their paper charts or don’t include information such as lab results if they don’t want to. I’m no longer shocked when practices ask me delete an item entered in error in their EMR. They do not want to see the item struck out, because back in the paper chart days, they just pulled it out and either discarded it or filed it elsewhere.
Striking out that information and noting the correction is the proper thing to do. Simply removing data from a chart has legal ramifications. It’s not the fault of the EMR software that these errors are now being pointed out to both clinic staff and their patients who request an e-copy of their chart or can see their chart on the clinic portal.
Many practices don’t address the underlying issues with their processes or their staff dynamics prior to implementation. It compromises the effectiveness and success of new EMR software processes. We are seeing widespread practice disintegration, and it is being blamed on the EMR software and the EMR vendors. However, the EMR is simply magnifying the existing dysfunction.
Before you throw out your EMR as the cause of all your new problems, consider that the problems already existed but were not visible in your hidden paper processes. Switching to another EMR is not going to solve your problems.
I recommend that all practices that are getting ready to implement EMR:
- Spend the time and money to have an outside party assess practice leadership, processes, and staff dynamics. Small practices will forego this suggestion because of cost, but productivity losses, staff turnover, and patient dissatisfaction will be more expensive in the long run. The return on investment will be created through greater efficiencies, cohesive staff, and better patient care.
- Document processes and enforce them from the top down. Everyone has to have skin in the game or it won’t work.
- Engage in team-building exercises to develop cohesion between all departments, including the physicians. These activities can be facilitated by an outside consultant, or they can be simple activities like bowling together. Bridge the existing rifts.
- Hold bottom-up staff meetings, allowing the staff to point out their issues and develop their own solutions. Empower them to build team alliances.
- Pay for extended onsite implementation support. I’m always shocked when an EMR vendor tries to make a deal by cutting implementation days to lower price. Three days to implement a new EMR with all-new processes, even for a one-doctor clinic, is a risky proposition.
- Define your leaders, empower them to make changes, and develop processes necessary for success. Allow them to lead you. The physicians should be falling in line along with their staff.
The key to a successful implementation and ongoing success of the practice is strong leadership. The person who was promoted from the front desk or billing office to the position of practice manager / administrator, likely does not have the leadership skills necessary to engineer this level of change management.
Invest in your leadership, send your managers for leadership training (or hire an experienced EMR project manager), and empower them to manage change in your practice. If the doctors aren’t willing to make changes, the staff won’t either be either, and your practice will suffer.
Julie McGovern is CEO of Practice Wise, LLC.




















Re: Walmart Health: Just had a great dental visit this morning, which was preceded by helpful reminders from Epic, and…